What Everyone Should Know About B-Type Natriuretic Peptide and Congestive Heart Failure
 By: by Amino Science
By: by Amino Science

Brain natriuretic peptide, commonly called B-type natriuretic peptide or, even more succinctly, BNP, is a hormone produced by the heart ventricles (the pumping chambers of the heart) in response to pressure changes linked to heart failure. Since its discovery in the late 1980s, it has earned a place of prominence in the medical world, as it can be used as a biomarker to facilitate the diagnosis of congestive heart failure (CHF).
Researchers have found that B-type natriuretic peptide measurements can be used not only to help with the diagnosis of heart failure, but also to predict future cardiovascular events and the risk that such events will prove fatal. This is part of what's known in clinical practice as risk stratification: the separation of patients into low risk, rising risk, and high risk in order to develop the most effective treatment plan possible.
According to an article published in Circulation, a journal published by the American Heart Association, BNP levels are "a powerful marker" for cardiovascular risk stratification. "In a recent study of 78 patients referred to a heart failure clinic, BNP showed a significant correlation to the heart failure survival score," the authors wrote. "In addition, changes in plasma BNP levels were significantly related to changes in limitations of physical activities and were a powerful predictor of the functional status deterioration." They mention, too, that measurements of BNP levels taken when patients came in through the emergency department could be used to predicate how patients would fare once they were discharged, with higher BNP levels strongly associated with worse prognoses.
There's some evidence as well that B-type natriuretic peptide concentrations have predictive value for other cardiac conditions, such as acute coronary syndromes and pulmonary embolism.
It's rare that a relatively new diagnostic measurement results in such rapid and widespread changes to clinical practice. Read on to learn exactly what B-type natriuretic peptide is and how measurements of BNP levels, which can be analyzed with a simple blood test, allow doctors to evaluate complicated elements of cardiovascular health.
What Is B-Type Natriuretic Peptide?
In scientific terms, B-type natriuretic peptide (BNP) is a polypeptide made of 32 different amino acids. When the muscles of the heart stretch excessively in response to changes in blood volume caused by heart failure, they release BNP along with its inactive, 76-amino acid synthetic byproduct, known as N-terminal prohormone BNP, or NT-proBNP.
BNP is one of four natriuretic peptides. All the members of this protein hormone family are secreted by components of the circulatory system. Atrial natriuretic peptide (ANP) is secreted by the atria of the heart (the upper pumping chambers), as its name indicates. BNP comes from the larger, stronger lower chambers, while C-type natriuretic peptide (CNP) is generated primarily in the blood vessels. The highest levels of dendroaspis natriuretic peptide, or D-type natriuretic peptide (DNP), the most recently discovered member of the family, have been found in blood plasma but are believed to be secreted by the heart.
All four natriuretic peptides appear to help regulate circulation. So far, experts have compiled the most data on the actions of ANP and BNP, which are jointly known as the cardiac natriuretic peptides. Both cause the blood vessels to dilate, allowing more blood to flow through them and lowering the risk of clot formation. They also help the kidneys flush out higher quantities of water as well as salt (a process called natriuresis).
Furthermore, researchers have found that ANP and BNP downshift the production of hormones like adrenaline, angiotensin, and aldosterone that narrow blood vessels, increase fluid retention, or elevate the heart rate.
The overall effect of the actions of ANP and BNP—namely, relaxing blood vessels, thereby lowering blood pressure, and improving renal function—ensures that the heart does not have to overtax itself. That's why when the heart is under stress, the body increases levels of these protective peptides.

How B-Type Natriuretic Peptide Relates to Heart Disease
As touched on in preceding sections, pressure changes inside the heart stimulate release of both B-type natriuretic peptide (BNP) and N-terminal (NT)-pro hormone BNP (NT-proBNP). Because those pressure changes tend to be indicative of either heart failure or some other type of cardiac malfunction, experts have proposed that both BNP and NT-proBNP levels might have prognostic value as a simple, inexpensive method of screening for cardiovascular diseases, particularly chronic heart failure.
The Effects of Chronic Heart Failure on the Body
Chronic heart failure, also called congestive heart failure (CHF), occurs when the ventricles (the walls of the heart chambers) become either too weak or too tense to properly pump blood throughout the body. Two of the top underlying causes are coronary artery diseases and high blood pressure. Other causes include heart valve diseases and, less frequently, diseases of the heart muscle (cardiomyopathies).
The heart's purpose is to draw in the blood that has been circulating through the veins and push it back out into the arteries. As the muscles weaken, the hearts of individuals with CHF cannot contract enough to fully pump blood back into the arteries. As a result, blood begins to collect in the lungs, then the veins, and the tissues of the body do not receive the supply of oxygenated blood they need.
Because of this lack of sufficient oxygen in their bodily tissues, individuals with CHF often feel fatigued and unable to exert themselves physically. Renal function becomes impaired—sometimes permanently—exacerbating the fatigue and making treatment more challenging. The brain suffers from this lack of oxygen-rich blood as well, causing confusion.
The blood collected in the lungs and veins produces its own set of symptoms, beginning with lung function. Shortness of breath is the definitive symptom of CHF. Initially, it only sets in during physical exertion, but as the disease progresses, it transpires while individuals are resting. Advanced CHF can make it impossible for individuals to sleep lying flat—when they do, their shortness of breath can intensify to the point where they are awakened by it. Other ways CHF shows up in the respiratory system include wheezing, coughing, and increased susceptibility to pneumonia. The most severe presentation is acute pulmonary edema, a buildup of fluid in the lungs that requires emergent medical attention.
Other symptoms of CHF include:
- Weakness
- Loss of appetite
- Fluid retention in the feet and legs
- Abdominal bloating
- Swelling of the scrotum and penis
- Frequent nighttime urination
- Diminished urine output throughout the day and night
- Weight loss (cardiac cachexia)
People of all ages can develop chronic, congestive heart failure—even children! Statistics show close to 5 million Americans currently have CHF, and around 555,000 new diagnoses are made each year.
This serious condition can be fatal, and it's common for death to occur suddenly. Individuals with CHF experience sudden death at a rate that's between 9 and 10 times that of the population at large! This makes it vital for doctors to have the means to rapidly and accurately diagnosis CHF.

Using B-Type Natriuretic Peptide to Diagnose Chronic Heart Failure
When it comes to diagnosing CHF in the advanced stages, doctors have a plethora of screening tests at their disposal. By that point, the symptoms will be quite clear, and chest X-rays, electrocardiograms (EKGs), or certain blood tests can confirm a doctor's suspicion.
Earlier presentations of CHF can be harder to catch, however, as symptoms overlap with those of a number of lung, liver, and kidney diseases. In order to determine the root cause of a patient's symptoms, doctors historically used an ultrasound test called an echocardiogram, or an echo for short. This safe, typically painless test allows doctors to see the heart muscles at work and to determine its ejection fraction, a measurement of the quantity of blood pumped by the left ventricle with each contraction. The healthy range for ejection fractions is between 50% and 70%.
The downside to echocardiograms is that they can be expensive and may not be available under all circumstances. This is where the value of BNP tests becomes clear. These simple, low-cost blood tests can be carried out bedside in an emergency department if need be. According to experts in the field, about 98% of the times that a BNP test reveals normal levels, it's accurate to rule out CHF as a diagnosis. This suggests to doctors that they should focus their attention on alternate explanations for shortness of breath or other symptoms that could indicate CHF.
At most facilities, a test revealing BNP levels below 100 picograms per milliliter (pg/ml) is grounds for eliminating CHF as a potential diagnosis. If patients are experiencing kidney failure, the threshold rises to 200 pg/ml.
When tests show high BNP levels, next steps become less certain. This alone does not fully support a CHF diagnosis, as there are other factors that can affect BNP levels, such as:
- Age
- Sex
- Lung, kidney, and liver health
- Blood pressure
- Thyroid function
- Cortisol levels
- Some uncommon tumors
- Brain hemorrhages
- Body weight
Certain medications, including diuretics, beta blockers, ace inhibitors, and spironolactone also impact BNP levels.
That said, BNP levels of around 900 pg/ml in individuals between the ages of 50 to 75, or over 1,200 pg/ml for those older than 75 correlate to a diagnosis of CHF 90% of the time. In most cases, patients with high BNP levels who do not have CHF have either severe lung or kidney disease.
BNP levels can not only help doctors make a diagnosis of CHF but also evaluate how far the disease has advanced, develop treatment plans, and determine how patients respond to different interventions. Generally speaking, the higher BNP levels are, the more severe the situation. As treatments take effect, backed up blood begins circulating into the rest of the body once again, and heart muscle cells begin to recover and to secrete less BNP.
A systematic review of clinical trials published in The BMJ looked at how accurate BNP measurements—both initial levels and changes in response to treatments—are for predicting risk of death, myocardial infarction (heart attack), and other cardiovascular events in heart failure patients. The authors determined that BNP has strong prognostic value for heart failure patients at all stages of the disease as well as for asymptomatic patients.
They went as far as to state that their findings raise "important questions concerning the way that heart failure is defined and diagnosed." The majority of the recent trials and studies they analyzed used ventricular systolic function, expressed in terms of ejection fraction measurements, as the reference standard for the diagnosis of heart failure. "This is despite the fact that it is recognized that 20-50% of patients with heart failure have preserved systolic function," they wrote. Given those statistics, they propose that BNP may be a superior method for identifying patients who would benefit from treatment for heart disease.

Can B-Type Natriuretic Peptide Levels Be Used to Diagnose Coronary Artery Disease?
When patients have coronary artery disease (CAD) without CHF, the muscles of their heart do not stretch in the way that spurs the release of BNP. If they have extensive coronary artery blockages, however, or active vascular inflammation, this can cause heart muscle cells to become ischemic (oxygen-deprived). Ischemic heart muscles cells also release BNP, though in smaller quantities than when they're attempting to counterbalance the effects of CHF.
Experts are quite excited about the possible use of BNP values to diagnose CAD, particularly for patients with asymptomatic CAD. As a review published in QJM: An International Journal of Medicine put it, "It would be of great benefit if a simple blood test could identify those most likely to have CAD." As a follow-up to that screening measure, individuals whose test results indicate they're likely to have CAD could undergo "more definitive but more invasive tests," like angiography and stress tests. The authors believe BNP testing "has the potential to reduce cardiac deaths" because its widespread use will let doctors "better target cardioprotective strategies to those who most need them."
What to Expect from a BNP Test
Now that you have a sense of why experts in the field of cardiovascular health find BNP tests almost endlessly exciting, you may be wondering, what exactly occurs during a BNP test?
As you know, the test measures BNP concentrations in the blood. In clinical practices, doctors are likely to recommend a BNP test when patients have symptoms of chronic heart failure like the classic shortness of breath. This simple, inexpensive test can catch CHF in the early stages before more serious complications develop. BNP tests can also be used to evaluate whether heart disease treatments are having the desired effects.
A BNP test does not require any special preparation, such as fasting. The test involves drawing blood from a vein using a hypodermic needle, so if you feel faint at the sight of blood, you may wish to ask a family member or friend to accompany you and drive you home.
The blood sample will then be sent to a laboratory where machines measure levels of BNP as well as NT-proBNP. This process typically takes between 15 and 20 minutes if the laboratory is located in the same facility where the test was performed. If the blood sample has to be sent to a separate laboratory, it make take up to a week for the results to be ready.
Once a doctor has reviewed the BNP test results, they will let you know whether your levels are high enough to indicate a diagnosis of heart failure. If you already have a confirmed diagnosis of CHF, your doctor will update you on whether your current treatment protocol is working effectively, as evidenced by lower BNP levels.
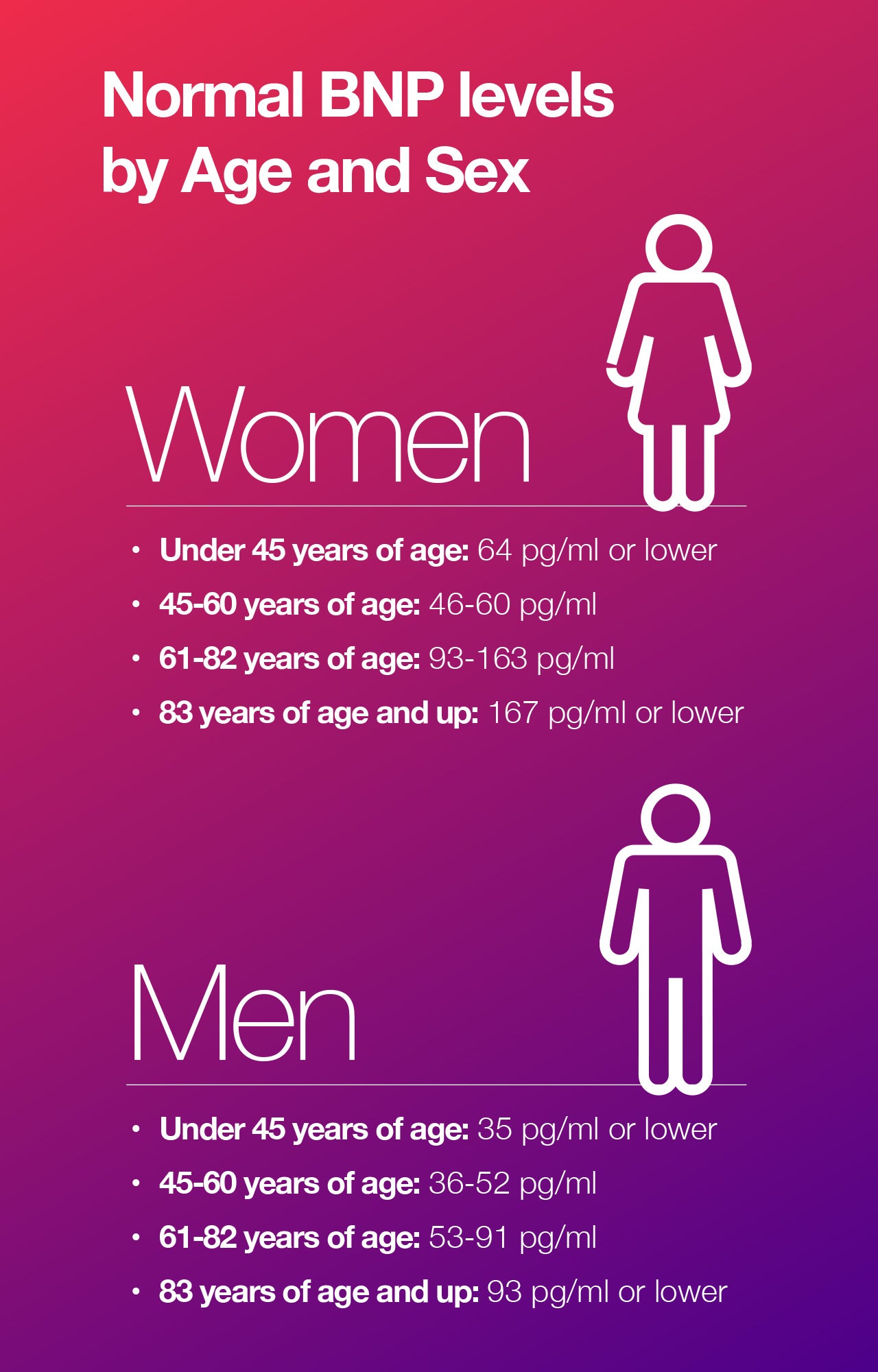
As touched on earlier, BNP levels under the threshold of 100 pg/ml usually exclude a diagnosis of heart disease. However, normal, healthy BNP levels fluctuate depending on your age and sex.
5 Expert-Approved Methods for Lowering BNP Levels
If you improve your heart health, your BNP levels will drop. Certain risk factors for heart disease are out of your control, such as a family history of the disease and your underlying genetic makeup. However, there are a variety of steps you can take on your own to address lifestyle-related risk factors known to negatively impact heart health, including:
- Stop smoking cigarettes. As you almost certainly know, smoking cigarettes harms your health. Studies have shown it undermines heart health in multiple ways, including raising your blood pressure, decreasing good high-density lipoprotein (HDL) cholesterol levels, and elevating your heart rate. It can be quite challenging to stop, but the benefits are undeniably worth the effort. After just 1 year, your susceptibility to heart disease drops significantly, and 15 years after cessation, it's equivalent to that of someone who has never smoked.
- Engage in regular physical activity. The Centers for Disease Control (CDC) recommend that adults get at least 2 hours and 3 minutes of moderate-intensity aerobic activity each week, along with at least two strength training sessions. If you find it difficult to fit exercise into your schedule, don't despair: even three 10-minute sessions daily can add up to make a difference. Try taking a brisk walk or spending time outside gardening. You can also build healthy habits into your day by taking the stairs, parking in the spot furthest from the door, or commuting to work on your bike. Ideally, you should also be finding ways to enhance your fitness by increasing the intensity, frequency, and duration of your workouts. Perform, Amino Co's athletic performance blend, can help.
- Prioritize stress management. Scientists have uncovered a clear link between uncontrolled stress and heart disease. The body responds to stress by releasing a hormone called cortisol, which can have a detrimental impact on your cardiovascular health. This is particularly true if stress becomes chronic. Be sure to find ways to manage the stress that inevitably arises as a part of life. Strong research supports the use of mediation and breathwork for this purpose.
- Get adequate sleep. Safeguarding your sleep is a vital part of stress management as well as the fortification of your overall health. Unfortunately, findings show that 30% of Americans experience intermittent insomnia, while many more struggle with milder forms of sleep deprivation on a regular basis. Building healthy sleep habits, such as refraining from working or eating in bed as well as using a computer or cell phone too close to your bedtime, can help you get the 7 to 8 hours experts advise for adults.
- Supplement with essential amino acids. As mentioned earlier, one of the physiological causes for chronic heart failure (CHF) is the weakening of the heart muscles. Researchers have found that amino acids can help counteract three of the ways that heart failure impairs muscle function: accelerated breakdown of muscle protein, poor regulation of muscle blood flow, and impaired production of cellular energy. Learn more about how to use essential amino acids to increase heart health here.


Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes



 833-264-6620
833-264-6620



















