HPV Vaccine for the Most Prevalent STI in America
 By: by Amino Science
By: by Amino Science

In 2006, the first HPV vaccine was approved for use in female and male children and young adults up to 26 years of age. The HPV vaccine has recently made headlines because the FDA has now approved its use up to the age of 45. But is this vaccine cocktail safe...or even necessary?
Before we explore HPV vaccine side effects and risks, let's get a better idea of what exactly the HPV virus is, and how it can affect our health.
What Is HPV?
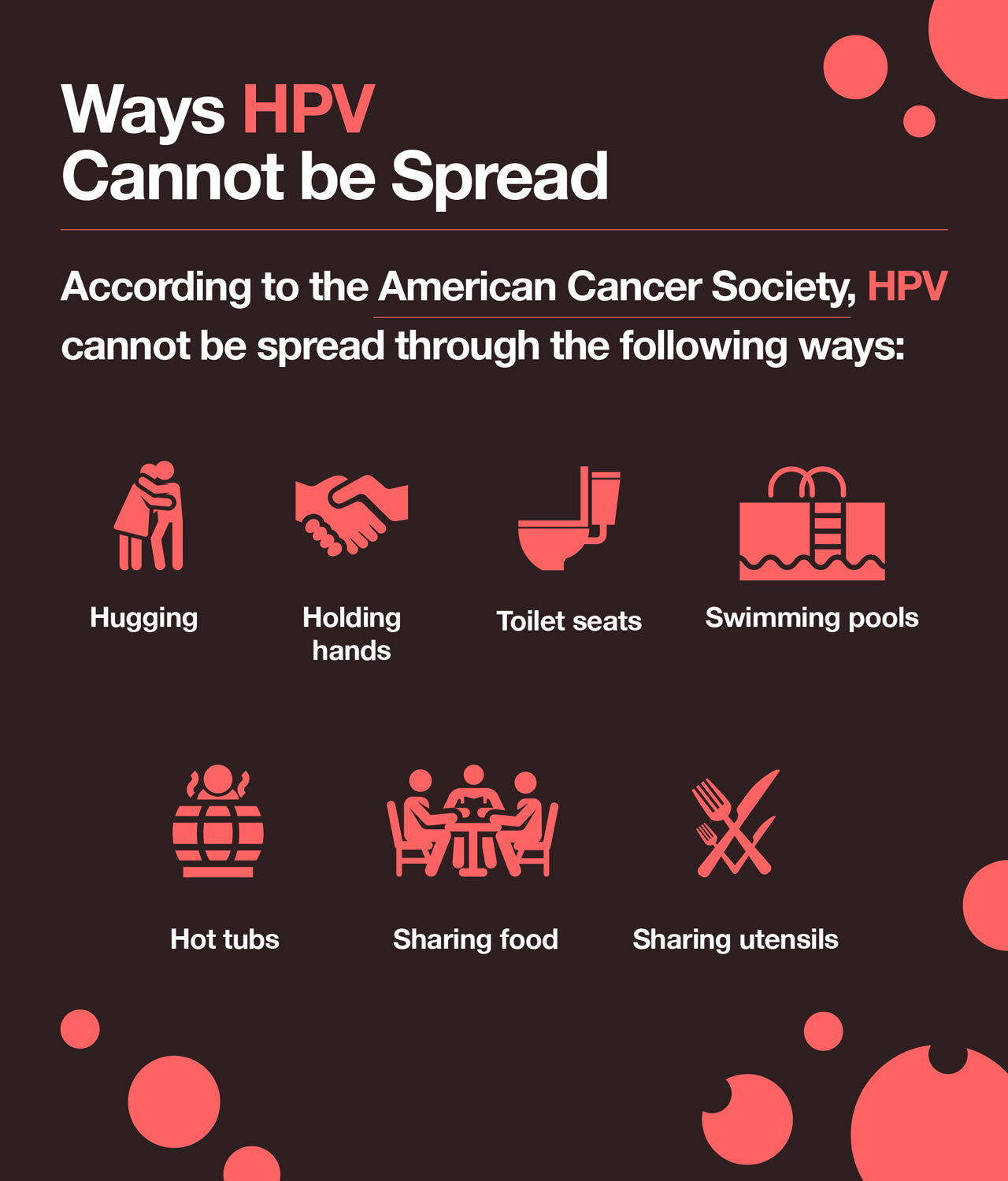
HPV is a sexually transmitted infection. It is spread through sexual contact such as touching, oral sex, and sex. Though it is most often spread through vaginal and anal sex, HPV can be spread in the absence of sex through intimate touching, rubbing, and grinding. Both men and women can contract and spread HPV, and most do at some point during their lifetimes. HPV viruses are so common that the Centers for Disease Control and Prevention (CDC) estimates that nearly all men and women will become infected with at least one type of HPV virus during his or her lifetime. According to the Know HPV website, there are 14 million new cases of HPV infection every year in the United States. That is approximately 19,000 people a day. The average age of those infected is 15 to 24.
HPV is an abbreviation for Human Papillomavirus. The name papillomavirus comes from the word papillomas. Papillomas are non-cancerous warts or tumors that may appear as a result of infection by some HPV viruses. HPV is not a single virus. Rather, it is a group of hundreds of viruses. According to the CDC, there are over 150 strains of HPV viruses.

Types of HPV and Their Symptoms
People who are infected with an HPV virus often don’t know that they have it. HPV viruses generally cause no signs or symptoms, which is one of the reasons HPV is so easily spread. People don’t have any symptoms to suggest something might be wrong so they don’t get tested.
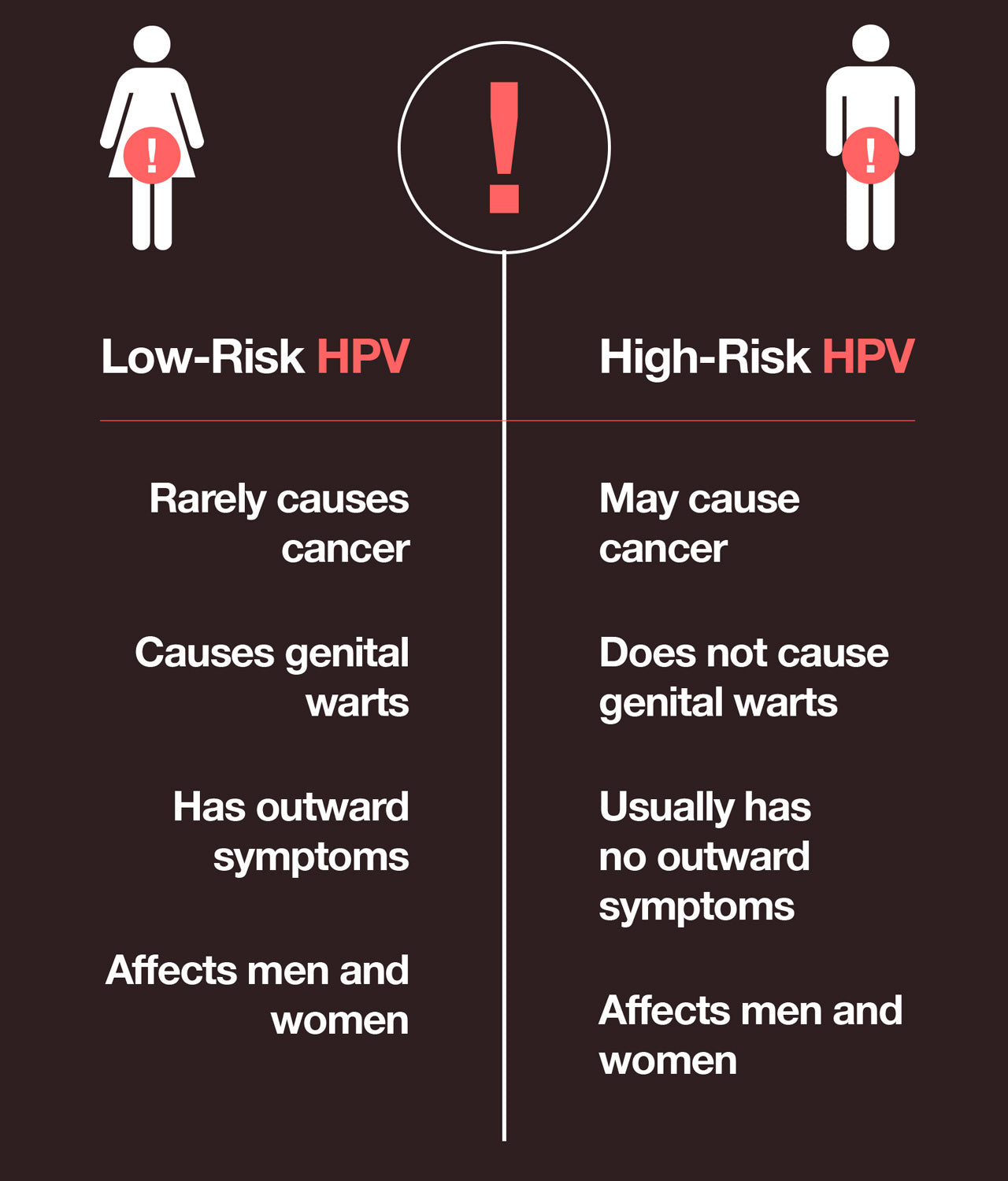
Each different strain of HPV is assigned a number. Some of the most common types of HPV are 6, 11, 16, and 18. Although there are over 100 different strains of the HPV virus, there are two main categories that these viruses fall into. They are High-Risk HPV and Low-Risk HPV. The symptoms and health risks vary for the two different types of the virus.
Low-Risk HPV
Low-risk HPV viruses rarely cause cancer, prompting the title “low-risk.” They do, however, cause outward symptoms such as genital warts that may appear weeks or even months after contracting the virus. This delay in symptoms is one of the reasons that HPV is so easily and quickly spread. Many people do not know they have it because they have no symptoms or symptoms do not appear right away. This also makes it difficult to pinpoint exactly when the virus was contracted and to understand how many others may have been exposed.
Most instances of genital warts are caused by HPV types 6 and 11. Genital warts from low-risk HPV in men may appear as tiny bumps around the genitals, including around the anus and on the penis. Low-risk HPV in women may cause genital warts around the anus and vagina. Sometimes, HPV warts can appear internally in places like the cervix, which needs to be viewed by a gynecologist. This is one reason why an annual well-woman exam is so important for women. Warts can also form on the hands and feet. Rarely, a condition called respiratory papillomatosis may occur, in which warts form in the respiratory tract and cause difficulty breathing.
High-Risk HPV
High-risk HPV viruses are the strains of HPV that are most likely to cause cancer. Over 31,000 cases of cancer each year are attributed to a type of HPV. Most HPV cancers are caused by HPV types 16 and 18. High-risk strains of HPV can cause cancer of the cervix, anus, vagina, vulva, penis, and the mouth, including the throat and tongue. High-risk HPV infections often have no outward signs or symptoms.
Most women find out they have HPV when they have a Pap smear as part of a regular gynecological exam. An abnormal Pap smear is an indication that something is not right with the cells on the cervix and usually prompts the physician to run an HPV test, which tests for the presence of the virus specifically. This is often when women find out that they are infected. Once a woman is diagnosed with HPV, it is critical that she receive regular Pap smear tests to watch for any cell changes that might indicate cervical cancer or even precancerous cells.
There is currently no routine HPV screening test recommended for men. So unless men have outward symptoms or are told by a sexual partner that they have been exposed to the virus, they likely will not be tested.
Is HPV Curable?
There is no cure for HPV. However, according to the CDC, most HPV infections go away on their own within two years of being contracted. HPV doesn’t always cause health problems and often goes away without the host ever realizing he or she had been infected. Other times, obvious symptoms such as genital warts occur.
So once it has been established that the virus is present, what is the next step? What treatment options are available?
HPV Treatment
If an HPV test is positive for low-risk HPV but there are no symptoms present, then treatment usually isn’t necessary. The CDC does not recommend the use of antiviral medications for HPV infections since the viruses often clear on their own spontaneously. However, if warts or an abnormal Pap smear are present, then treatment is available. For those with low-risk HPV, genital warts can be treated with creams and removed by a physician. For women with high-risk HPV, Pap smears can detect changes in cervical cells that may lead to precancerous or cancerous conditions. Regular Pap smears allow doctors the chance to monitor cell changes and proceed as necessary should cancer become a serious concern. In some cases, a procedure called Loop Electrosurgical Excision Procedure (LEEP) may be performed in which precancerous cells and tissue are removed from the cervix and vagina.
HPV Prevention
For those not yet sexually active or those who have tested negative for HPV, preventative measures such as condoms should be considered to avoid contracting HPV in the future. Condoms are not guaranteed to protect against HPV, as there is still a chance of skin-to-skin contact occurring. But condoms can help reduce the chances of contracting HPV as well as other sexually transmitted infections. For those who have already contracted HPV, condoms should still be used in the hopes of preventing it from spreading. Even if there are no outward symptoms of HPV, such as an active outbreak of genital warts, HPV can still be spread through contact with an infected person.
It's always a good idea to keep the immune system strong with supplements such as essential amino acids.
HPV Vaccine
There is an HPV vaccine available, recommended by the CDC for boys and girls as young as 11 or 12. The Gardasil 9 vaccine is given as a series of two or three shots usually in the arm. Gardasil 9 protects from nine different types of HPV viruses including Types 6, 11, 16, 18, 31, 33, 45, 52, and 58. The majority of HPV-related cancers can be attributed to these nine types of HPV. Those who were not vaccinated as children or teenagers are also recommended to get the vaccine. The recommendation used to be specifically for men and women up to age 26, but, as previously mentioned, the FDA has approved the use of the HPV vaccine up to age 45.
HPV Vaccine Schedule
The Advisory Committee on Immunization Practices (ACIP) advises the following HPV vaccine schedule:
- For adolescents: Two doses of the HPV vaccine 6-12 months apart before the 15th birthday.
- 16 and up (or those with immunocompromising conditions): Three doses of the HPV vaccine. The second dose should be administered one to two months after the first, with the third following at month six.
Is the HPV Vaccine Recommended for Boys and Men?
The HPV vaccine for boys is recommended at age 11 or 12, which is on schedule with CDC recommended vaccines for meningitis and whooping cough. It can, however, be administered as early as age nine.
The CDC recommends the HPV vaccine for men who have sex with other men, or who have compromised immune systems, such as men with HIV. The recommended cutoff age used to be 26, but has been extended to age 45.
HPV Vaccine Side Effects
HPV can be prevented by practicing safe sex and choosing your partners wisely. If you do choose to safeguard with the HPV vaccine, then it's wise to weigh the vaccine against its numerous side effects. The most common HPV vaccine side effects are:
- Pain, swelling, itching, bruising, redness, bleeding, or a prominent lump at the injection site.
- Headache
- Fever
- Dizziness
- Tiredness
- Diarrhea
- Sore throat
- Generalized abdominal pain
- Fainting
More severe reported HPV vaccine risks include:
- Anaphylaxis
- Appendicitis
- Asthma
- Blood clot in the extremities
- Bronchospasm
- Cellulitis
- Guillain-Barre Syndrome
- Inflamed spinal cord
- Inflammation of the stomach and intestinal linings
- Life-threatening allergic reaction
- Low platelet count and bleeding
- Lung embolism
- Multiple sclerosis induced by Gardasil
- Obstruction in a blood vessel caused by a blood clot
- Pancreatitis
- Pelvic inflammatory disease (PID)
- Seizures
- Transverse myelitis
- Venous thromboembolic events
These HPV vaccine side effects and risks can manifest in a matter of hours, days, weeks, or months. If you suffer from any of the aforementioned symptoms, consult a doctor right away.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes



 833-264-6620
833-264-6620



















