What Is Hydrocephalus? Plus Causes, Symptoms and Prognosis
 By: by Amino Science
By: by Amino Science

Hydrocephalus, the accumulation of excess fluid around the brain, can affect infants, children, and adults. In infants and young children, the most obvious symptom tends to be a rapid increase in head circumference, or, if hydrocephalus is present from birth, an atypically large head. Older children and adults present with different symptoms, as their skulls cannot expand to make room for the buildup of fluid. While hydrocephalus causes remain somewhat mysterious, the condition can be treated, though doing so requires surgery. While prognosis after treatment varies, it's entirely possible for individuals to recover and go on to experience a good quality of life.
What Is Hydrocephalus?
The medical term hydrocephalus, derived from Greek, is somewhat misleading. The word hydro means water in Greek while the word cephalus means head. Despite the fact that hydrocephalus was historically referred to as "water on the brain," the accumulated liquid that's characteristic of this condition is not water at all. It's cerebrospinal fluid. The purpose of cerebrospinal fluid (CSF) is to surround and protect the brain as well as the spinal cord, however, a delicate balance of this fluid must be maintained.
CSF has three absolutely vital functions:
- Act as a cushion for brain tissue, protecting it from jostling and blows
- Transport nutrients and waste
- Offset changes to intracranial blood volume by moving between the cranium and the spine
When all is working as it should, CSF flows through the ventricular system (four spaces in the brain linked by narrow passages), spills into the cisterns located below the brainstem (which essentially act as reservoirs), travels across the exterior of the brain and spinal cord, and then enters the bloodstream where its reabsorbed.
The body continuously produces CSF, so if any element of the system malfunctions, causing the flow of CSF to be disrupted, it will begin to accumulate in the ventricles. As the ventricles widen to accommodate the buildup of fluid, excessive pressure is placed on the tissues of the brain. That pressure on the brain, in turn, causes hydrocephalus.

Differentiating Between Types of Hydrocephalus
Per a fact sheet prepared by the National Institute of Neurological Disorders and Stroke (NINDS), a division of the National Institutes of Health, diagnoses of hydrocephalus fall into one or more of the following categories.
1. Congenital Hydrocephalus
When hydrocephalus is diagnosed at birth, it's called congenital hydrocephalus. This type of hydrocephalus develops due to either genetic abnormalities or to events or environmental factors present during gestation.
2. Acquired Hydrocephalus
Any type of hydrocephalus that is not present at birth is deemed acquired hydrocephalus. This type of hydrocephalus can develop during infancy, childhood, or adulthood. It occurs as a result of diseases or injuries that affect the brain.
3. Communicating Hydrocephalus
This type of hydrocephalus describes presentations of the condition in which the normal flow of CSF stops after it leaves the ventricles. This means CSF can still move through and between the ventricles themselves.
4. Non-Communicating Hydrocephalus
Non-communicating, or obstructive, hydrocephalus (as you might be able to intuit) refers to conditions in which CSF cannot pass through one (or more than one) of the passages linking the ventricles. For example, in one type of non-communicating hydrocephalus, called aqueductal stenosis, the accumulation of CSF results from constriction of the aqueduct of Sylvius, which links the third and fourth ventricles at the center of the brain.
5. Hydrocephalus Ex-Vacuo
This form of hydrocephalus, which primarily occurs in adults, results from brain damage caused by strokes or traumatic injuries. This presentation differs somewhat from those described so far and is characterized primarily by the shrinking of brain tissue.
6. Normal Pressure Hydrocephalus
Known causes of normal pressure hydrocephalus (NPH) include head trauma, subarachnoid hemorrhages, tumors, infections, or surgical complications. However, it's also possible for this type of hydrocephalus to transpire without the presence of a single one of the factors listed above. The highest rates of NPH are found among older adults. According to the NIH, approximately 375,000 older Americans develop NPH. The Hydrocephalus Association puts that number even higher, stating that a recent study found up to 700,000 older Americans may have NPH, with 80% of those cases going undiagnosed and untreated.

What Causes Hydrocephalus and Who Is at Risk?
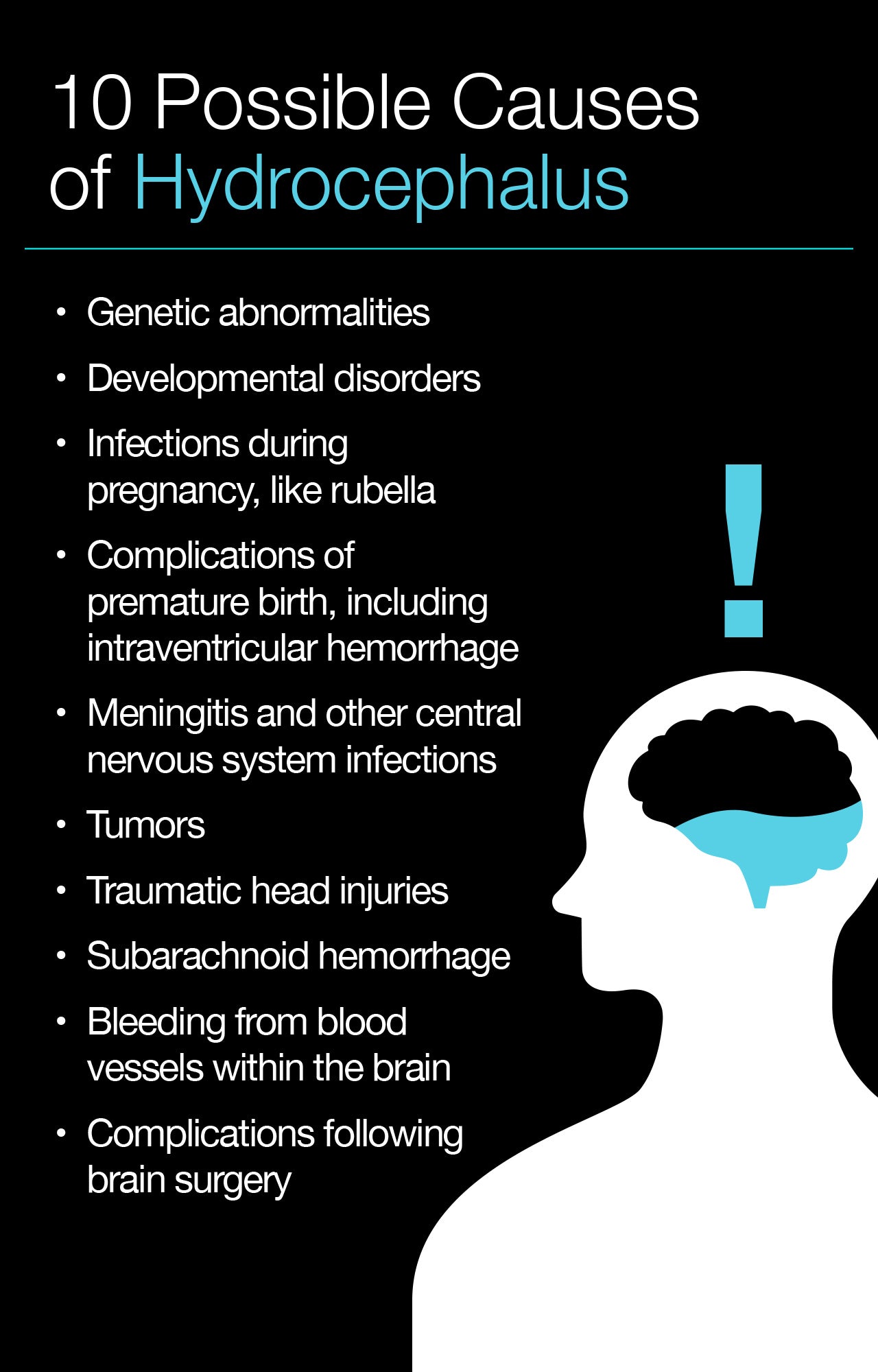
In the simplest terms, hydrocephalus happens because a blockage interrupts the normal flow of CSF, the ability of your blood vessels to absorb CSF becomes compromised, or the brain begins to produce more CSF than it needs. Some common causes of hydrocephalus have already been described in the preceding section. Yet all in all, the instigating factors that result in hydrocephalus remain somewhat obscure. So far, researchers have identified the following potential triggers:
- Genetic abnormalities
- Developmental disorders
- Infections during pregnancy, like rubella
- Premature birth complications, including intraventricular hemorrhage
- Meningitis and other central nervous system infections
- Tumors
- Traumatic head injuries
- Subarachnoid hemorrhage
- Bleeding from blood vessels within the brain
- Complications following brain surgery
It can be challenging to determine how many people develop hydrocephalus annually or currently have this condition, especially given the potential for NPH to go undiagnosed. According to the Hydrocephalus Association, around 1 million Americans have hydrocephalus.
This condition affects people of all ethnicities, income levels, and stages of life. That said, it's most common in infants and in adults age 60 and above. Statistics indicate that between 1 and 2 out of every 1,000 babies born have congenital hydrocephalus, making it just as prevalent as Down's syndrome and more prevalent than both spina bifida and brain tumors. The NIH fact sheet mentions a review published in the Journal of Neurosurgery: Pediatrics in 2008 which found that hydrocephalus accounted for 1.8% of all pediatric hospital days and 3.1% of all pediatric hospital charges in the United States. It's also the single most common reason children have to undergo brain surgery.
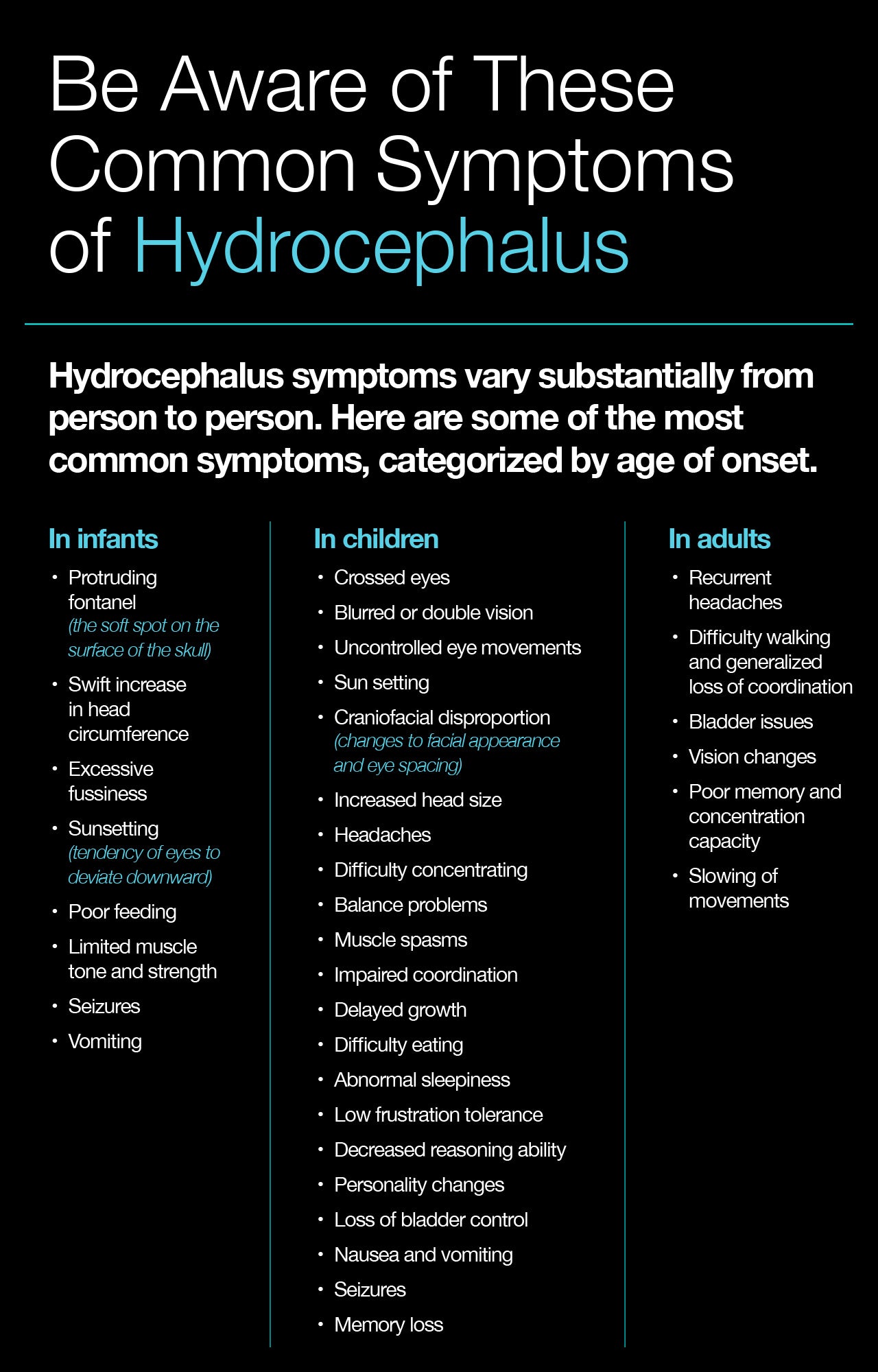
Recognizing Common Symptoms of Hydrocephalus
Because hydrocephalus can cause permanent brain damage, it's extremely important to seek medical attention promptly. In order for that to happen, you must be able to recognize the symptoms of hydrocephalus. This can be a bit tricky, as symptoms shift depending on a person's age at onset, how far the disease has progressed, and individual variations that impact response to fluid buildup. As an example of this, when hydrocephalus develops in an infant, their skull can adjust in response to increased CSF pressure and widening of the ventricles by expanding since the sutures (fibrous joints connecting the bones of the skull) remain open.
Here are symptoms of hydrocephalus to look for, categorized by age at onset.
Infancy
- Protruding fontanel (the soft spot on the surface of the skull)
- Swift increase in head circumference
- Excessive fussiness
- Sunsetting (tendency of eyes to deviate downward)
- Poor feeding
- Limited muscle tone and strength
- Seizures
- Vomiting
Childhood
- Crossed eyes, double vision, or blurred vision
- Uncontrolled eye movements
- Sun setting
- Craniofacial disproportion (changes to facial appearance and eye spacing)
- Increased head size
- Headaches
- Difficulty concentrating
- Balance problems
- Muscle spasms
- Impaired coordination
- Delayed growth
- Difficulty eating
- Abnormal sleepiness
- Low frustration tolerance
- Decreased reasoning ability
- Personality changes
- Loss of bladder control
- Nausea and vomiting
- Seizures
- Memory loss
Adulthood
- Recurrent headaches
- Difficulty walking and generalized loss of coordination
- Bladder issues
- Vision changes
- Poor memory and concentration capacity
- Slowing of movements
It's important to note that the symptoms of normal pressure hydrocephalus, which frequently occurs in older adults, overlap with those of other disorders like Alzheimer's disease. When a patient presents with symptoms such as urinary incontinence, difficulty walking, and increasingly worse memory, doctors are far more likely to suspect dementia than hydrocephalus. This leads to high rates of improperly diagnosed as well as undiagnosed cases of normal pressure hydrocephalus.
It should also be said that while the symptoms listed above cover the most common presentations of hydrocephalus, this condition presents differently each time it occurs.
Diagnosing Hydrocephalus
To evaluate a patient who may have hydrocephalus, a doctor will first conduct a thorough physical exam. Pediatricians in particular use this to check for a larger-than-normal head circumference, bulging fontanel, and slowed reflexes.
When evaluating an infant whose fontanel has not yet closed, a pediatrician may use ultrasound to examine the brain by bouncing high-frequency sound waves off of it to create images.
Other tests used to diagnose hydrocephalus include:
- Neurological examination
- Computed tomography scan (CT scan)
- Magnetic resonance imaging (MRI)
- Lumbar puncture, also known as a spinal tap
- Lumbar catheter
- Monitoring of intracranial pressure
Clinicians select the most appropriate test or tests based on a patient's age, symptoms, and the known presence or indication of irregularities of the brain or spinal cord.
Treating Hydrocephalus
Without proper treatment, hydrocephalus can be fatal. While treatment may not allow for the reversal of brain damage that has already ensued, it can ensure that no more occurs by reestablishing a normal flow of CSF.
At this time, no medical therapy exists for the treatment of hydrocephalus—the only available options are surgical. In most cases, treatment of hydrocephalus involves conducting a surgery to insert a shunt system that allows CSF to travel out of the central nervous system and into another part of the body where reabsorbtion can occur during the normal process of circulation.
A shunt system is relatively simple in design and concept. It involves just three components: a strong, flexible tube called a shunt, a thin tube called a catheter, and a valve. During surgery, a neurosurgeon situates one end of the catheter either inside the brain itself or in the areas around the spinal cord where CSF circulates. The surgeon then places the other end of the catheter in a location where the CSF can drain and be absorbed. Typically, this is in the abdominal cavity, though the areas surrounding the lungs or heart chamber can also be viable options. The valve, located along the catheter, controls the direction and rate of CSF flow. A shunt system will typically need to remain in place throughout a person's life and will require close monitoring.
A far less common treatment option is what's called an endoscopic third ventriculostomy. During this surgical procedure, the surgeon uses a device called a neuroendoscope (a tiny camera) to view the surface of the ventricles. Once they have guided the scope into position, allowing them to examine this small, difficult-to-access surgical area, they use an instrument to create a very small opening in the bottom of the third ventricle. In cases where this would be a good treatment option, the hole then allows CSF to flow unobstructed into the area of reabsorption surrounding the brain's surface.

Life After Hydrocephalus
Given the number of variables involved in the development, progression, and treatment of hydrocephalus, it's difficult to generalize about outcomes. Factors that impact a person's prognosis include:
- Underlying cause
- Rapidity of diagnosis
- Presence of related disorders
- Degree of relief of CSF pressure
The success of shunt surgery and ventriculostomy vary quite a bit from person to person. Taking an essential amino acid supplement optimized for surgical recovery can help improve rehabilitation outcomes. In general, the earlier hydrocephalus is diagnosed and treated, the more complete a person's recovery will be.
It's important for those affected by hydrocephalus as well as their families to understand that this condition can affect cognitive as well as physical development. After surgery has been performed, treatment and management should be guided by an interdisciplinary team that includes rehabilitation specialists. When connected with the right rehabilitation therapies, individuals diagnosed with this condition can lead independent lives with few restrictions.
Unfortunately, fewer than 10 medical centers in the United States currently specialize in the treatment of this condition, according to the Hydrocephalus Association. Because it involves so many variables and unknowns, doctors who do not specialize in the condition can be reluctant to take on complicated hydrocephalus cases. This means that not everyone with hydrocephalus will be able to access appropriate care.
There has also been limited progress over the last half-century in terms of identifying more effective treatments for hydrocephalus or methods of prevention. "Research is essential," states the Hydrocephalus Association. "At the very least, we need better treatments, with more positive long-term outcomes, and diagnostic tests that are accurate, cost-effective, and noninvasive."
At this time, the bulk of the research that's done is in the pediatric space. The Hydrocephalus Clinical Research Network (HCRN) is made up of seven pediatric medical centers that analyze data from all their hydrocephalus patients with the aim of more rapidly identifying treatment improvements. This collaborative research effort not only carries out concurrent studies at all seven centers, but also oversees an extensive database of patient histories and procedures.
The work of the HCRN, as well as other research efforts focused on hydrocephalus, are supported by the NINDS, along with other institutes of the NIH. While the primary goal of these endeavors is to uncover ways to treat, prevent, and cure hydrocephalus, researchers also investigate the immensely complicated mechanisms underpinning brain development with the hope of understanding more about the origins of neurological conditions.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















