IBS vs. IBD: What’s the Difference Between These Two Bowel Conditions?
 By: by Amino Science
By: by Amino Science

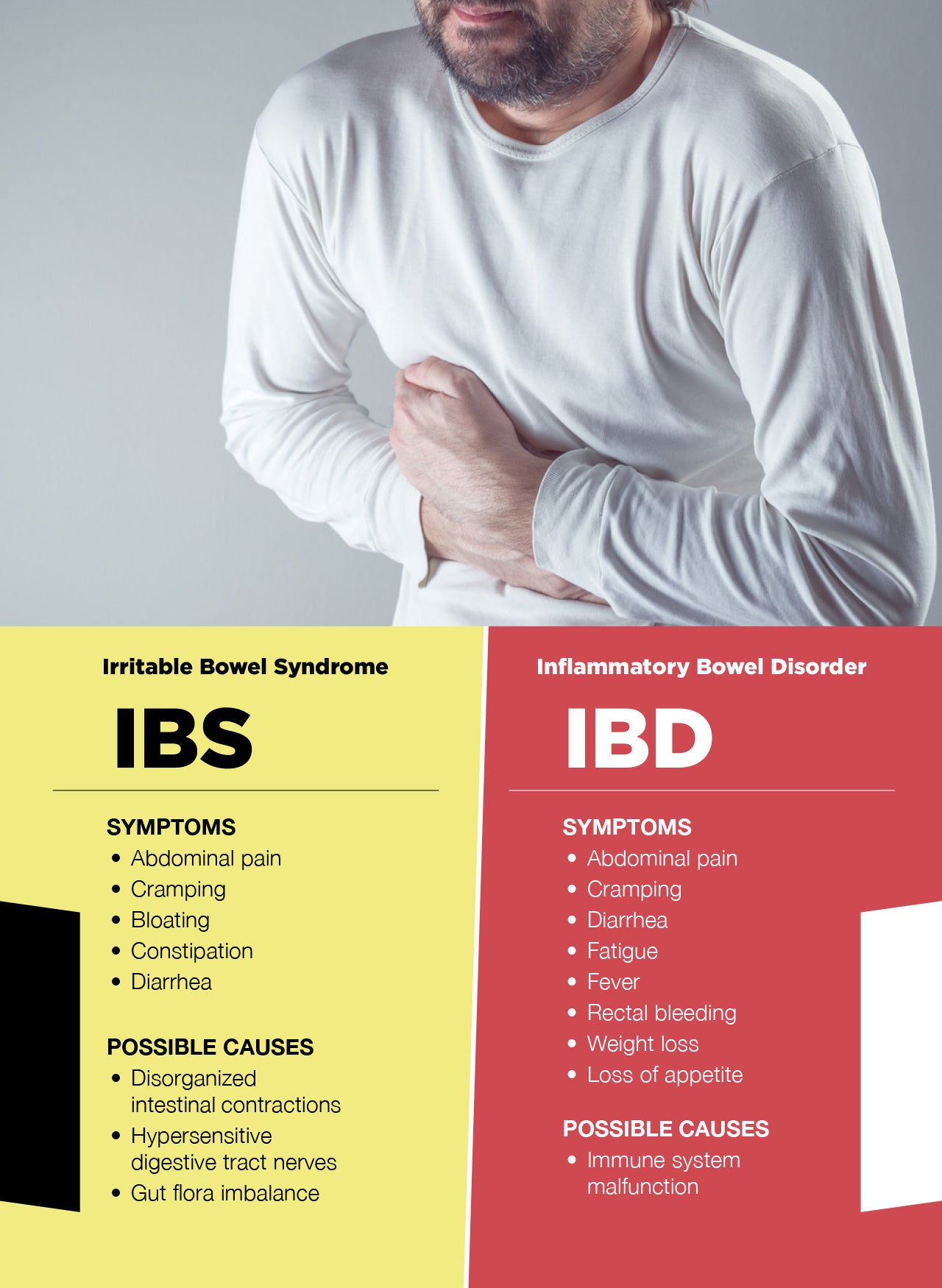
Irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) are medical conditions that share some similar symptoms and for this reason are sometimes confused with one another. However, IBS and IBD are two distinct disorders with different causes and treatments. So if you’re struggling with symptoms and wondering if it’s IBS or IBD, come with us as we explore the similarities and differences as well as common symptoms and treatment options for each.
What Is IBS?
IBS is a functional disorder of the large intestine that affects the way the colon works. While the precise cause of IBS remains unclear, certain factors appear to play a role in the condition. These include:
- Disorganized intestinal contractions: The muscles that line the intestines usually contract smoothly to move food along the digestive tract, but in people with IBS, these movements become disorganized and can be weak (as in IBS with constipation predominance, or IBS-C) or overly forceful (as in IBS with diarrhea predominance, or IBS-D).
- Hypersensitive nerves: People with IBS may have abnormalities in the nerves of the digestive tract that cause the colon to overreact to normal digestive processes. Moreover, there’s increasing evidence to suggest that alterations in levels of the neurotransmitter serotonin (most of which resides in the gut) may be involved as well.
- Gut flora imbalance: Studies suggest that people with IBS may have altered levels of good vs. bad bacteria in their intestines.
Most people with IBS experience mild symptoms that can be controlled with simple lifestyle and dietary changes. However, some individuals may have symptoms severe enough to interfere with their day-to-day lives. Common symptoms of IBS include:
- Abdominal pain
- Cramping
- Bloating
- Constipation
- Diarrhea
Symptoms of IBS can also be triggered by things like stress, certain foods, and fluctuations in hormones, such as those seen during menstrual periods. Certain risk factors may also predispose an individual to IBS. These include:
- Age: People under the age of 50 are more likely to develop IBS.
- Sex: Women are twice as likely as men to have IBS.
- Family history: People with family members with IBS are more likely to develop the condition themselves.
- Psychological history: People with a history of anxiety, depression, or childhood trauma may have a greater risk of developing IBS.
What Is IBD?
IBD is a term used to describe a group of digestive diseases of the gastrointestinal tract—or GI tract—that involve chronic inflammation. The two most common types of IBD are ulcerative colitis, which affects the innermost layer of the large intestine and rectum, and Crohn’s disease, which may involve the entirety of the intestinal lining throughout the digestive system. Common IBD symptoms include:
- Abdominal pain
- Cramping
- Diarrhea
- Fatigue
- Fever
- Rectal bleeding
- Weight loss
- Loss of appetite
Like IBS, the precise cause of IBD is unknown, but it’s thought that people with the condition may experience an abnormal immune response in the presence of invading pathogens—a response that causes the immune system to attack healthy cells in the digestive tract.
Certain risk factors are also thought to influence the development of IBD. These include:
- Race/ethnicity: Caucasians and people of Ashkenazi Jewish descent are more at risk of developing IBD.
- Family history: People with a close family member with IBD have a greater risk of developing the condition themselves.
- Tobacco use: People who smoke have a higher chance of developing Crohn’s disease, though smoking appears to result in a decreased risk of ulcerative colitis.
- Nonsteroidal anti-inflammatory drugs: People who use NSAIDs like ibuprofen, naproxen, and celecoxib have a higher chance of developing IBD or experiencing worsening of pre-existing symptoms.
IBS vs. IBD: The Takeaways
As you can see, there are a number of similarities as well as differences between IBS and IBD. Perhaps the biggest difference, though, is the fact that IBS is a functional gastrointestinal disorder and IBD is an inflammatory disorder. In other words, while the symptoms of IBS can be attributed to a disturbance in the functioning of the GI tract, the symptoms of IBD are the result of an actual disease process.
In addition, IBS doesn’t cause any damage to the digestive system, though people with severe symptoms may have a decreased quality of life. By contrast, people with IBD have a greater risk of developing serious complications, including:
- Joint, skin, and eye inflammation
- Colon cancer
- Liver damage
- Blood clots
- Bowel obstruction or perforation
Finally, while the number of Americans with IBD is estimated to be around 1.4 million, IBS is thought to affect approximately 25 to 45 million people in the United States.
IBS vs. IBD: Treatment Dos and Don’ts
Just like we’ve seen in our discussion of symptoms, the treatments needed to address IBS and IBD have some overlap as well, but there are some important differences that should also be kept in mind.
Treating IBS
As discussed earlier, the majority of people with IBS can manage their symptoms by following a few simple lifestyle and dietary guidelines.
Foods that commonly trigger symptoms of IBS include spicy foods, cruciferous vegetables like broccoli and cabbage, caffeinated and carbonated beverages, citrus fruits, and beans.
In addition, a 2012 study found that diets low in the fermentable oligosaccharides, disaccharides, monosaccharides, and polyols—or FODMAPs—found in some grains, vegetables, fruits, and dairy products may be beneficial for some people with IBS.
However, diets that contain plenty of probiotics and fiber, especially soluble fiber—which studies have found can help regulate bowel motility and feed good gut bacteria—have been shown to aid in symptom relief. Studies have also shown that the use of both peppermint and fennel, which have been found to reduce colonic spasms and decrease abdominal pain, bloating, and gas, can be beneficial in the treatment of IBS.
Stress management that emphasizes proper sleep as well as techniques such as exercise, meditation, yoga, and tai chi is also recommended. And because more and more evidence is identifying a link between serotonin and IBS symptoms, people who struggle with IBS-D may benefit from supplementing with the serotonin precursors L-tryptophan and 5-hydroxytryptophan (5-HTP).
Treating IBD
Because IBD is a serious disease that can lead to long-term and even life-threatening complications if not properly addressed, the main goal of treatment is reducing the inflammation that underlies the condition. Therefore, IBD treatment usually begins with medication, including:
- Anti-inflammatory medications: Depending on the affected portion of the GI tract, patients with mild to moderate IBD symptoms may be prescribed anti-inflammatory drugs such as corticosteroids or aminosalicylates. While corticosteroids are used as short-term therapy during flare-ups, aminosalicylates can be utilized for long-term treatment.
- Immunosuppressants: These types of medications help suppress the immune system’s release of the chemicals known to damage the cells of the GI tract.
- Antibiotics: These medications are used in cases where IBD has led to an infection or required surgery.
Although there’s currently no evidence firmly linking stress to IBD, many people who suffer from the condition have noted a direct correlation between increased stress and symptom flare-ups, so IBD patients may benefit from using stress reduction techniques.
The link between diet and IBD is also not clear, but certain foods and beverages can aggravate symptoms. For this reason, experts recommend keeping a food diary to track foods that help and foods that harm.
For example, many people with IBD experience symptoms after eating spicy, fatty, or fried foods or dairy products or after drinking alcohol or carbonated or caffeinated beverages. High-fiber foods may also aggravate symptoms, as may cruciferous vegetables, nuts, seeds, and popcorn.
Additional dietary and lifestyle habits that may improve symptoms of IBD include:
- Water: Drinking plenty of water can help stave off dehydration and prevent the overstimulation of the GI tract that can lead to diarrhea.
- Small meals: Eating five or six small meals a day, as opposed to two or three large ones, can help people with IBD avoid the overstimulation of the digestive tract that may lead to symptoms.
- Supplements: IBD can interfere with the body’s ability to absorb nutrients, so vitamin and mineral supplements may be a helpful addition to the diet. Likewise, iron supplements may be required if IBD results in bleeding and associated anemia. In addition, a 2017 study found that even though there’s a possible link between diets high in animal protein and the development of IBD, there’s also evidence to suggest that supplementing with amino acids may actually have beneficial effects on the digestive system.
If diet and lifestyle changes and medications aren’t successful in treating IBD, surgery will likely be recommended. In the case of ulcerative colitis, symptoms may be completely eliminated by removing the entire colon and rectum and forming a pouch that attaches the small intestine to the anus—or creating an opening in the abdomen for use with a colostomy bag.
People with uncontrolled Crohn’s disease may undergo multiple surgeries to remove damaged parts of the digestive tract, drain abscesses, or repair abnormal connections (fistulas) caused by ulcers. Unfortunately, as many as 50% of people with Crohn’s disease require surgery at some point, yet because of the extensive nature of the condition, surgery may provide only temporary relief of symptoms.
If you or someone you love is experiencing symptoms that point to the possibility of IBS or IBD, be sure to seek medical advice from your health care provider. Dealing with either of these conditions can bring up a lot of questions and concerns. But your health care provider can assist you in finding the guidance you need to help control your symptoms and improve your quality of life.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















