What Are Opioids? America’s Opioid Crisis
 By: by Amino Science
By: by Amino Science

The opioid crisis is a public health calamity that has profoundly crippled America’s economic well-being and social order. According to the Centers for Disease Control and Prevention (CDC), opioid use, which includes prescription and illicit opioids, has lead to more than 350,000 overdose deaths since the late 1990s, while drug overdose deaths continue to increase. An average of 115 Americans die each day from opioid overdose. The aggregate loss of life due to opioids has been so devastating that it has contributed to recent declines in the nation’s life expectancy rate.
The misuse of prescription opioids alone has placed a tremendous strain on the United States economy. A loss of $78.5 billion a year accounts for criminal justice costs, health care expenditures, loss of productivity, and addiction treatment expenses. Even worse, the U.S. Council of Economic Advisers’ (CEA) recent report concerning the economic toll of the opioid crisis suggests that previous cost estimates grossly undervalued fiscal losses due to opioid overdose fatalities.
The Makings of a Crisis
The opioid crisis started in the 1990s when health care providers began prescribing opioids—a group of pain-relieving pharmaceuticals—to pain sufferers at substantially higher rates than in years past. A sharp rise in overdose deaths materialized as a result.
Years later in 2010, overdose deaths from heroin use rose. The National Institute on Drug Abuse estimates that 4% to 6% of people who succumb to prescription opioid misuse eventually switch to heroin, while 80% of individuals who use heroin first abused prescription opioids.
The year 2013 is the most recent major benchmark in the opioid crisis that saw yet another marked increase in overdose deaths—this time mostly from the use of synthetic opioids, illicitly-manufactured fentanyl (IMF) in particular. The U.S. Department of Health and Human Services reports that in 2016, an astounding 2.1 million people misused prescription opioids for the first time.
The opioid crisis has affected all areas of the United States, but its social, economic, and public health impacts have been most noticeable in rural areas of the country. The National Institute on Drug Abuse highlights that the Midwestern region saw a 70% rapid increase in opioid overdoses from July 2016 through September 2017. Meanwhile, opioid overdoses have surged tremendously by 54% in large cities in 16 U.S. states.
Now that doctors and health institutions have been made aware of the high risk of substance use disorder from opioid prescriptions, addicts who find it difficult renewing their prescriptions or increasing their dose often turn to illicit measures to acquire heroin, illegally-dispensed opioid medication, or highly-lethal synthetic opioids that are usually more addictive versions laced with contaminants. Unsupervised drug use and increased criminal activity linked to peddling and acquiring opioids have further worsened the opioid crisis, affecting both users and non-users while burdening social and health institutions in diverse communities across America.
Opioid Addiction Causes
Opioids are drug substances that have been around for centuries. They are derived from the opium poppy, or breadseed poppy, plant of the family genus Papaveraceae. In the 4th century BCE, opioids were used for religious, recreational, and medicinal purposes. In the 19th century, the opioid morphine was a popular pain medication and cough suppressant. Medicinal and recreational use of the opium poppy derivative heroin began shortly thereafter. Synthetic opioids were designed in the 20th century. Today, most opioids are considered controlled substances—meaning there is a possibility of dependence and misuse.
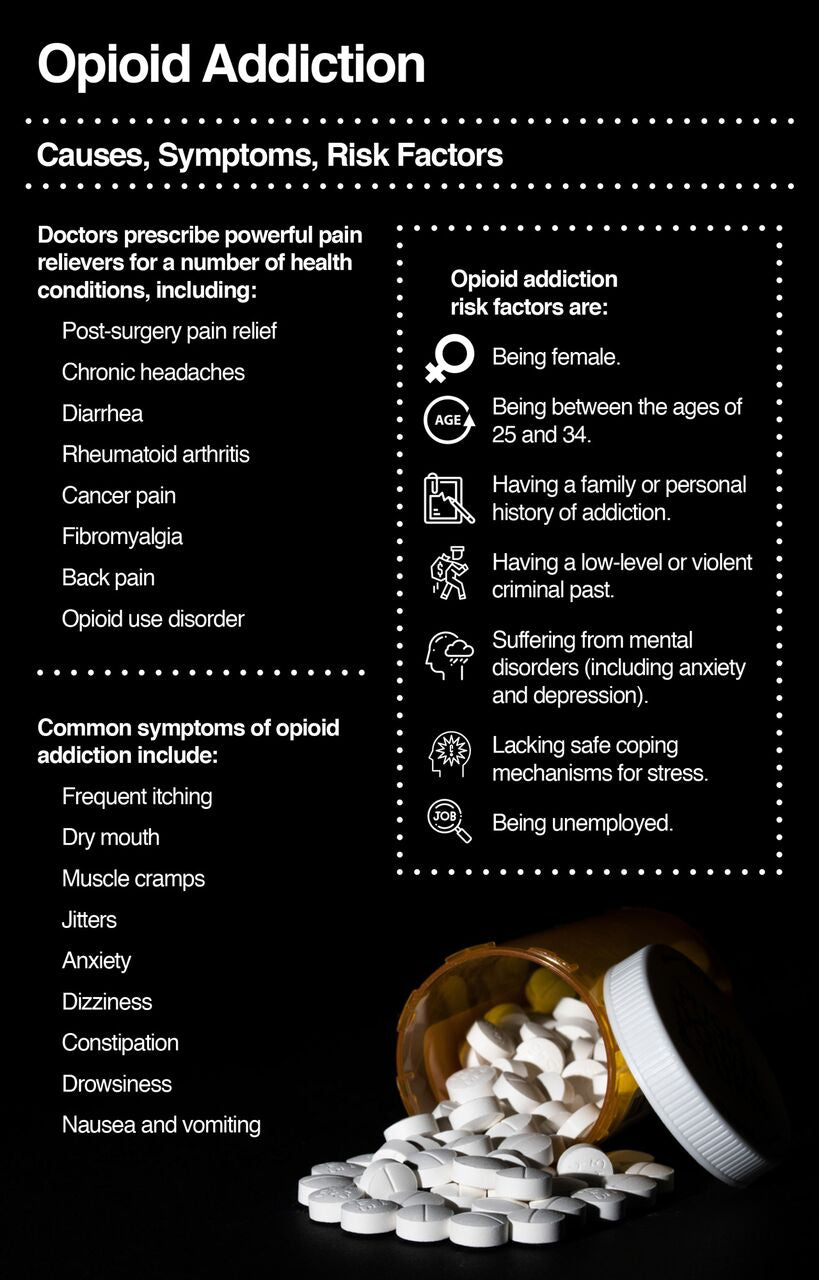
While heroin is illegal, natural and synthetic opioids may be prescribed for restricted medicinal use. Doctors have prescribed powerful opioid pain relievers for a number of health conditions, including:
- Post-surgery pain relief
- Chronic headaches
- Diarrhea
- Rheumatoid arthritis
- Cancer pain
- Fibromyalgia
- Back pain
- Opioid use disorder
What Are Opioids?
Pharmaceutical companies offer a wide variety of opioids available in prescription form, or in low-potent over-the-counter medications (e.g., codeine). Hydrocodone, hydromorphone, oxycodone (OxyContin), meperidine, methadone, naloxone, and fentanyl are common pain relievers that are usually reserved for moderate to severe pain. Doctors prescribe most of these prescription drugs in pill form. Fentanyl is available in patch form.
When a patient takes opioids, the brain releases endorphins, which are “feel-good” neurotransmitters. Endorphins disrupt how we perceive pain, as they induce strong, though ephemeral, euphoric feelings in the body. When the effects of the opioid wear off, unimpeded pain perception returns and may heighten during opioid use. The user feels compelled to retake opioids to numb pain and to experience a state of pleasure.
Opioid addicts often report that subsequent repeated drug abuse stems from their pursuit of the same euphoric effects they felt during their first opioid experience. However, as opioid tolerance increases, higher doses are necessary to attain euphoric effects which have likely diminished in strength. Nevertheless, without strict medical intervention addicts continue to pursue the same potency levels of pleasure by misusing opioids, which usually escalates to addiction.
Common symptoms of opioid addiction include:
- Frequent itching
- Dry mouth
- Muscle cramps
- Jitters
- Anxiety
- Dizziness
- Constipation
- Drowsiness
- Nausea and vomiting
Patients taking opioids under a doctor’s strict supervision may also experience these symptoms. It is very important to speak with you doctor before starting any pain medication. Be sure to discuss pharmaceutical and non-drug alternatives to opioids as well.
Opioid Addiction Risks
A number of national task forces, which were formed to combat the opioid crisis, continue to assess reasons why opioid addiction is so prevalent in the United States.
As is the case in many states throughout the country, South Dakota has seen a sharp rise in opioid deaths since the early 2000s, but the state’s mortality rate due to opioid overdose deaths was lower in 2016—5 deaths for every 100,000 persons—than the national average, which was 13.3 opioid overdose deaths for every 100,000 persons for the same year. Through funding from the CDC, South Dakota’s Department of Health formulated the Opioid Abuse Advisory Committee that monitors the state’s opioid epidemic. The committee found that inadequate health coverage, poverty, and limited access to mental health services increase opioid addiction risk.
A 2002 report published in the journal Addiction Science & Clinical Practice points to environmental abnormalities that may further the biological components of addiction, including: stress, psychological conditioning, social circumstances surrounding the first opioid use, and genetic predisposition pertaining to brain structure even before the first dose of opioid is taken.
It has been widely suggested that risk of opioid use increases if opioids are prescribed for non-cancer chronic illness treatment. Doctors should exercise caution when prescribing opioids for patient use longer than 3 to 5 days for non-cancer care. After 5 days, the likelihood of patient opioid use for a year or patient misuse of opioids increases.
Snorting or injecting crushed opioid pills or combining opioids with other medications increases the risk of addiction and accidental overdose death. For example, misuse of fentanyl—an extremely potent opioid—combined with other opioids substantially increases risk of death.
Here is a list of other typical opioid addiction risks:
- Gender: Females experience chronic pain more than men, and thus are prescribed opioids at higher rates. Women are often prescribed higher doses than men, and take opioids for longer durations of time.
- Age: Adults between the ages of 25 and 34 have higher rates of overdose deaths than other age demographics. In 2016, 129 out of every 100,000 suffered an opioid-related death.
- History: Individuals with a family history of addiction or who themselves have suffered addiction in the past are more susceptible to opioid addiction. People with a low-level or a violent criminal past are at high risk of addiction.
- Psychological problems: People who suffer mental disorders (including anxiety and depression) have fewer safe coping mechanisms for stress, or they may not seek adequate treatment but instead self-medicate with illicit drugs like opioids.
- Unemployment: Those who are unemployed may experience a disruption in health insurance or funds necessary for proper and consistent medical treatment. Furthermore, the stress of unemployment can aggravate or induce depression and anxiety.
Opioid Side Effects
Some individuals who were first prescribed opioids to treat pain and become addicted may experience a rare condition known as opioid-induced hyperalgesia—where they experience more pain as a result of the same medication. Opioid-induced hyperalgesia most often occurs when doses are rapidly increased. Repeated opioid use over time and increased opioid doses can lead to:
- Chronic drug addiction
- Overdose death due to respiratory depression
- Tolerance and dependence
- Heighten sensitivity to stress
- Neonatal abstinence syndrome (for babies of mothers who have used opioids during pregnancy)
- Spread of infectious diseases (e.g., HIV, hepatitis C) among substance abuse populations due to unsanitary conditions, needle sharing, etc.
Opioid Crisis Intervention
State and federal health, research, and social institutions are fighting the opioid crisis in several key areas. Prevention is the best way to stave off opioid addiction, especially in at-risk populations. The CDC funds states with resources to best monitor opioid-related overdoses in order to develop evidence-based addiction and overdose prevention methods that include consumer awareness training for patients and pain management education for health providers. Collaborative data-collecting and policing measures among state and federal agencies are strongly encouraged in order to identify social circumstances that may exacerbate the opioid crisis.
In recent years, the U.S. Department of Health and Human Services (HHS) and the National Institutes of Health (NIH) have bolstered resources for research in the areas of pain management and the biological mechanisms associated with opioid addiction. At the onset of the opioid crisis, many scientists instinctually focused opioid investigation resources on exploring the correlation between amino acid neurotransmitters and opioid receptors in the brain. Such a centered focus in opioid research has lead to the development of antagonist drugs that respond to the same brain structures and processes as addictive opioids, but with preservative and normalizing effects.
Medical facilities and first responders utilize the popular opioid overdose drug naloxone to help counter opioid overdoses. Other antagonist drugs like buprenorphine and methadone are utilized during opiate substitution therapy (OST) to manage the biological effects of addiction and to help facilitate safe opioid withdrawal. In addition to biological remedies, psychosocial treatments can help opioid patients manage the stressors of everyday living with the hopes that rehabilitation may encourage recovering addicts to become healthy, functioning members of society. Nutritional therapies such as essential amino acid supplements can help keep neurotransmitters balanced in the brain.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes


 833-264-6620
833-264-6620