Breaking the Silence Around Male Infertility
 By: by Amino Science
By: by Amino Science

While fertility problems can affect both men and women, male infertility (sometimes called male factor infertility) tends to get less attention. However, research shows that 35% of the time when couples suffer from infertility, the underlying issues have to do with the male partner. And with around 13% of couples experiencing infertility at one time or another, men who wish to have children may find it necessary to undergo infertility testing.
To further understanding of male infertility, we'll be covering symptoms and causes of male infertility, tests used to diagnose male infertility, and common treatment options for fertility issues in men.
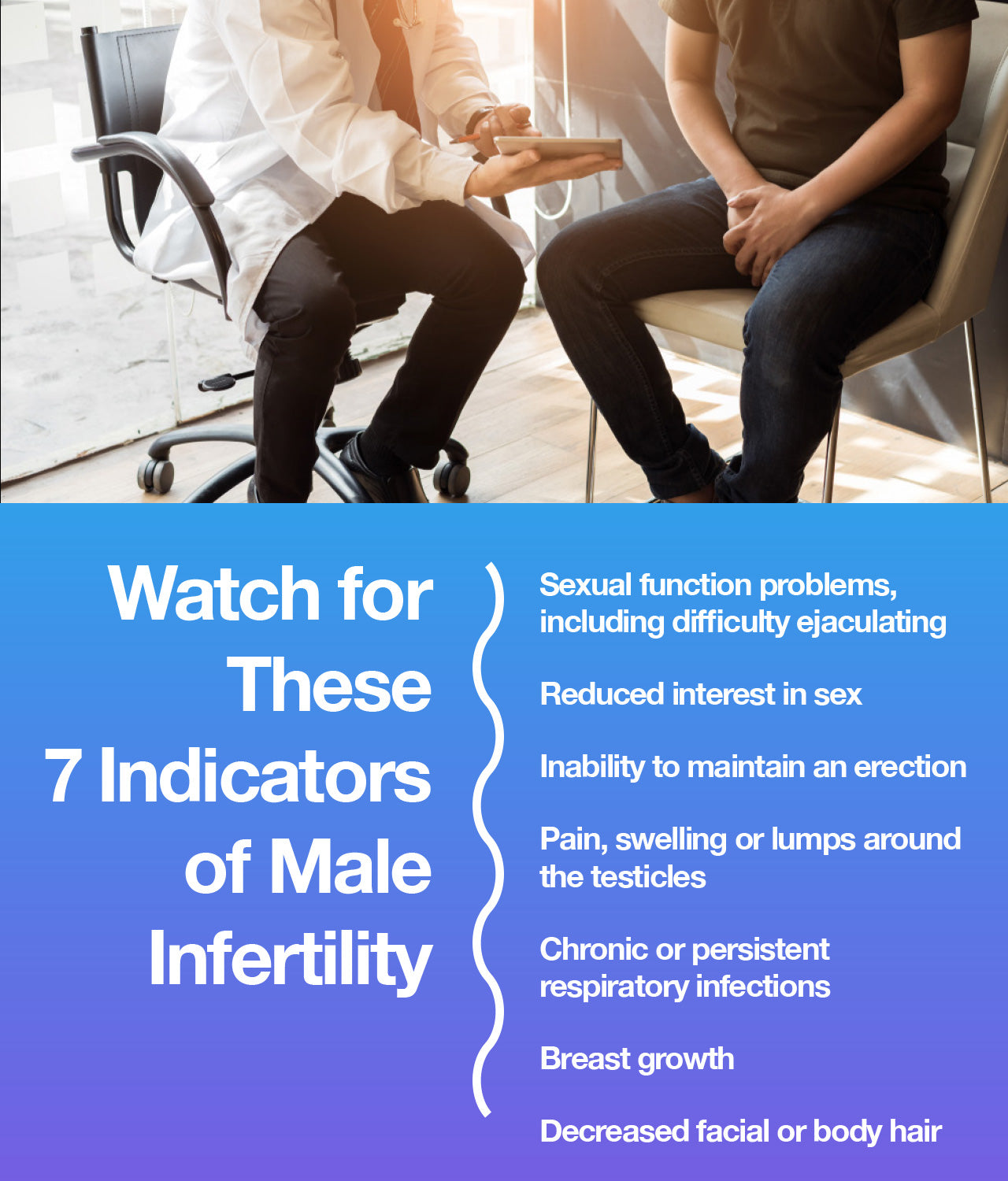
7 Symptoms of Infertility in Men
Before covering some common indicators of male fertility issues, let's go over the functions of the male reproductive system under normal conditions.
Sperm production, storage, and transportation are the primary responsibilities of the male reproductive system. In order for mature, healthy sperm to be produced, there must be appropriate levels of hormones present—in particular, the male sex hormone testosterone.
Both sperm production and testosterone production occur in the testicles. Sperm then travel to tubes located just behind the testicles called the epididymides. Just prior to ejaculation, sperm move from the epididymides to another set of tubes, the vas deferens, which wrap around the bladder to link up with the ejaculatory duct from the seminal vesicles.
When ejaculation occurs, sperm mix with fluid from the prostate and seminal vesicles to form semen, which then moves through the urethra and out of the penis. Successful fertilization occurs when the sperm travels through a female partner's vagina, passes through the cervix and uterus into the fallopian tubes and links up with an egg.
Many factors can interfere with healthy male fertility; however, unlike some other medical conditions, infertility in men doesn’t typically result in a lot of noticeable symptoms. That said, some possible indicators of male infertility include:
- Sexual function problems, including difficulty ejaculating
- Reduced interest in sex
- Inability to maintain an erection
- Pain, swelling, or lumps around the testicles
- Chronic or persistent respiratory infections
- Breast growth
- Decreased facial or body hair
If you or your partner has been trying to get pregnant for a year without success, it may be time to see a doctor to discover the cause of your fertility difficulties.
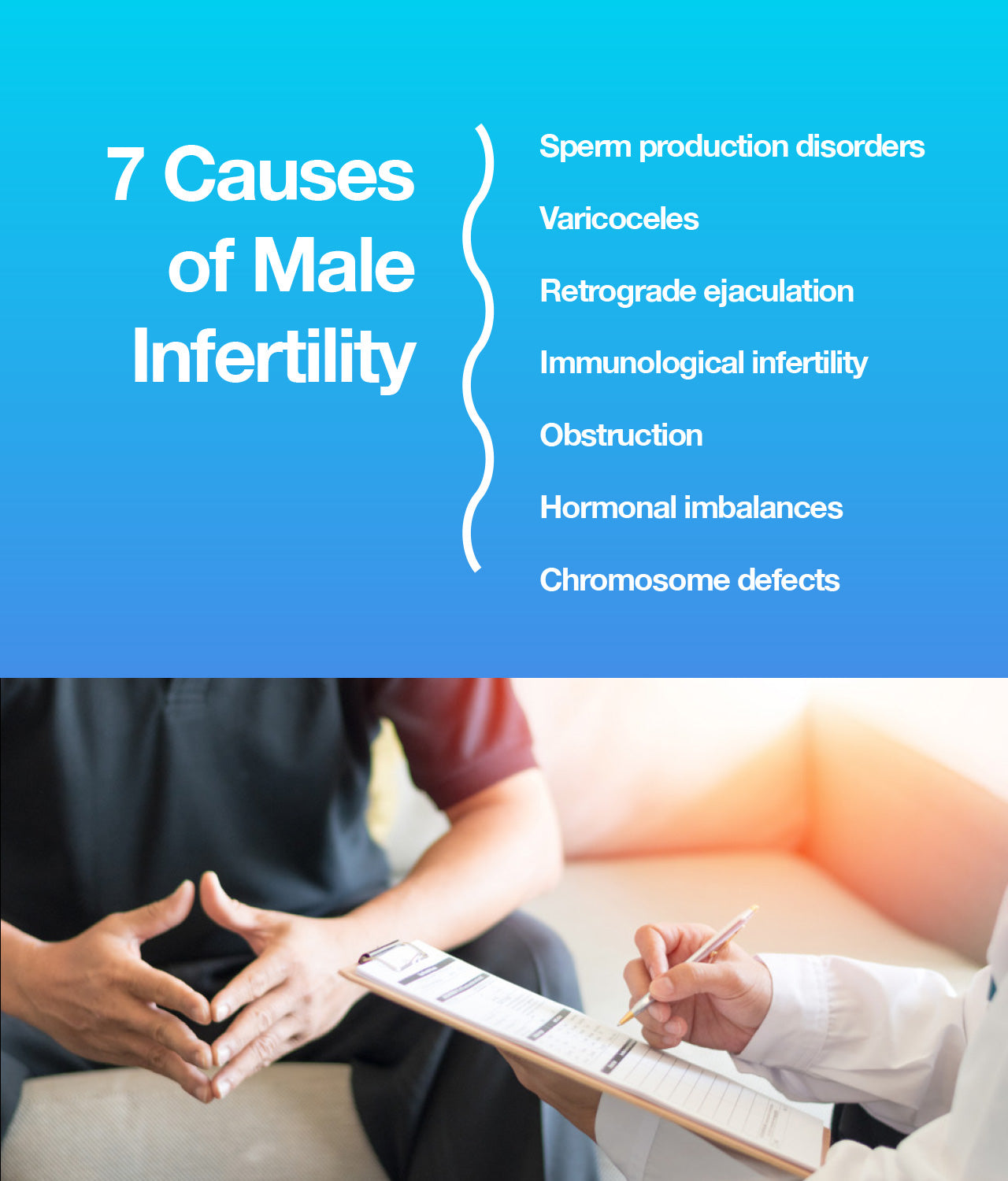
What Causes Male Infertility?
There is no single cause of infertility in men. The male reproductive system is quite complex and multiple prerequisites must be in place to guarantee healthy sperm function. Issues can arise that prevent cells from developing into sperm, or prevent sperm from traveling to their biologically programmed destination. Even a seemingly innocuous and constantly fluctuating factor such as the temperature of the scrotum can affect male fertility.
The best way to identify and resolve fertility issues is to speak with a professional in the field of reproductive medicine. That said, the underlying causes of male infertility can be grouped into the following 7 categories.
1. Sperm Production Disorders
The causes of infertility in men often relate to issues with sperm production. This category encompasses multiple fertility issues, from issues with sperm development to low sperm count and beyond.
In some cases, men produce a completely adequate number of sperm, but the sperm themselves are oddly formed, not fully grown, or unable to move well. In others, men may learn they have oligospermia, meaning they produce sperm in low numbers, resulting in an overall low sperm count, or azoospermia, meaning the levels of sperm in their semen are undetectable.
Sperm disorders can be genetic, but they can also be the product of lifestyle choices such as drinking or smoking cigarettes, or a side effect of certain medications. Other potential causes of low sperm counts include chronic illness such as kidney disease, childhood infections including the mumps, and hormonal imbalances.
2. Varicoceles
A varicocele is a medical term used to describe an enlarged vein in the scrotum. A fairly common condition—found in about 16 out of every 100 men—that typically develops during puberty, varicoceles can interfere with sperm production by preventing proper blood drainage. This can lead to lower sperm count as well as lower sperm quality. It can also shrink the testicles.
Varicoceles does not always impair fertility, but they are more common in infertile men (the rate of diagnosis climbs to 40 out of 100). Doctors have not yet identified risk factors for developing a varicocele. It's also not entirely clear why varicoceles impact fertility. Some theories include that they cause blood to flow back into the scrotum from the abdomen, which causes the temperature in the scrotum to rise. This is a known cause of low sperm count.
In many cases, varicoceles present with no accompanying symptoms. If symptoms do appear, they include a lump in one of the testicles, scrotal swelling, visibly enlarged or twisted veins in the scrotum, and a dull, recurring pain in the scrotum.
3. Retrograde Ejaculation
Retrograde ejaculation is a condition in which when semen travels backward into the body. Rather than exiting the penis, they slide into the bladder. The semen may contain healthy, normal sperm, but since it does not exit the man's body, it cannot fertilize an egg. This condition is not innately harmful, and typically only requires treatment in order to resolve accompanying fertility issues.
The primary symptom of retrograde ejaculation is orgasms in which a man ejaculates very little or no semen. These are sometimes referred to as dry orgasms. A secondary symptom is urine that's cloudy after orgasm because it contains semen.
During a male orgasm, sperm travels through the vas deferens to the prostate to mix with other fluids to form semen. A muscle at the opening of the bladder called the bladder neck muscles contracts to keep semen from entering the bladder as it passes from the prostate into the urethra. For individuals experiencing retrograde ejaculation, the bladder neck muscles fail to tighten and semen can move into the bladder rather than being ejaculated from the penis.
Underlying causes of retrograde ejaculation include:
- Surgery: Procedures affecting the male reproductive system, such as bladder neck surgery, prostate surgery, or surgery to treat testicular cancer, can result in retrograde ejaculation.
- Certain medications: Some drugs used to treat high blood pressure, prostate enlargement, and depression can cause side effects that bring about retrograde ejaculation.
- Chronic conditions: Certain conditions that cause nerve damage, including diabetes, multiple sclerosis, Parkinson's disease, or a spinal cord injury, can also lead to retrograde ejaculation.
4. Immunologic Infertility
Although this is not a common cause of male infertility, it's nonetheless a crucial one to address. In certain circumstances, a man's body can begin to generate antibodies that attack his own sperm.
These antisperm antibodies are immune cells that mistakenly view sperm to be harmful invaders and work to protect the body from that perceived threat. Antisperm antibodies typically result from injury, surgery, or infection. It appears that they lower fertility by making it more difficult for sperm to travel to the fallopian tube and fertilize an egg.
5. Obstruction
It's also possible for male infertility to be caused by a physical blockage. Repeated infections, surgical complication, swelling, or congenital conditions can damage the male reproductive system and cause obstructions to develop.
Any part of the male reproductive tract can be blocked. With a blockage in place, even healthy, fully-functioning sperm are unable to exit the body during ejaculation, and therefore unable to successfully fertilize an egg.
Experts estimate that for approximately 4 out of every 10 men with azoospermia, the underlying issue is an obstruction that blocks sperm from traveling through the reproductive tubes.
6. Hormonal Imbalances
Anything that affects the hormonal systems—including the hypothalamus, pituitary, thyroid, and adrenal glands—can adversely impact male fertility. The pituitary gland produces hormones that regulate sperm production, including testosterone. When testosterone levels drop, sperm decreases as well.
Low testosterone levels (which doctors call male hypogonadism) and other hormonal problems may stem from a variety of underlying causes, such as:
- Injury to the testicles: Physical injury to both testicles as well as some cancer treatments can damage the testicles, causing testosterone levels to fall.
- Pituitary disorders: These can be caused by drugs, kidney failure, or small tumors.
- Kallmann syndrome: This condition has been linked to abnormal hypothalamus function and altered hormone levels.
- Inflammatory diseases: Illnesses such as tuberculosis, sarcoidosis, and histiocytosis can impact the pituitary gland and the hypothalamus, thereby impacting hormone levels.
- HIV/AIDS: This virus can can affect the pituitary gland, hypothalamus, and testes.
7. Chromosome Defects
Researchers have found that chromosomal anomalies and genetic mutations account for between 10% and 15% of all male infertility cases.
Klinefelter's syndrome—in which a male is born with two X chromosomes and one Y chromosome (instead of one X and one Y)—is one of the most common known causes of male fertility issues. This condition causes men to have smaller testes, lower testosterone levels, and decreased sperm production. Typically, men with this condition must seek out fertility treatments in order to biologically father children.
Another direct cause of male infertility, Y chromosomal infertility occurs in 1 out of every 2,000 men. Men with this condition have genetic deletion in the Y chromosome, which impacts protein production, which in turn causes low sperm production, the production of abnormally shaped sperm, or halts sperm production altogether.
The above list is not intended to be comprehensive, but rather to give an overview of the complexity of the male reproductive system and the many factors that can impact male fertility.
As we've touched on in some of the preceding sections, it's even possible for medications to change sperm production, function, and delivery. Health problems for which these medications might be prescribed (and which have not been referenced previously) include arthritis and digestive problems, as well as:
- Infections
- High blood pressure
- Cancer
And in some rare cases, male infertility can result from celiac disease.
Diagnosing Male Infertility
An initial male fertility examination includes a comprehensive medical history, physical examination, general hormone tests, and one or more semen analyses.
According to resources made available by the University of California, San Francisco, this is what to expect when consulting a doctor about male infertility.
Medical History
The goal here is to identify any elements in a person's medical history that may be contributing to their fertility issues. To do so, a doctor will typically cover the following areas:
- Medications
- Prior surgeries
- Any family history of infertility or birth defects
- Lifestyle factors such as smoking and drinking
- Occupational hazards such as exposure to potentially harmful substances
Physical Exam
After completing the medical history, doctors usually conduct a thorough physical examination. The focus here will be on the pelvic organs: the penis, testes, prostate, and scrotum.
The physical examination is especially helpful when it comes to diagnosing varicoceles.
Semen Analysis
After collecting semen in a sterile cup, doctors can study it to look for issues with volume, count, concentration, motility, shape, structure, and volume and liquidity of ejaculate.
Equipped with all that information, doctors can begin pinpointing whether a patient is suffering from an issue with the seminal vesicles, a blocked ejaculatory duct, and so on.
Other Laboratory Testing
Doctors may use blood tests or other laboratory testing to help determine the underlying cause.
Two of the tests a doctor is most likely to order at an initial visit are urinalysis and hormonal tests. A urinalysis can indicate the presence of an infection, while hormonal tests provide a measure of testosterone levels and FSH (follicle-stimulating hormone). If initial tests indicate it, serum LH and prolactin tests may be ordered too.
If it's not possible to make a diagnosis after the initial evaluation, further tests may be required, such as:
- Seminal fructose test: This test identifies whether the seminal vesicles are properly adding fructose to the semen.
- Post-ejaculate urinalysis: This test can determine if obstruction or retrograde ejaculation is occurring.
- Semen leukocyte analysis: This test shows if there are white blood cells in the semen.
- Kruger and World Health Organization (WHO) morphology: This form of analysis focuses on sperm shape and features.
- Antisperm antibodies test: This test looks for antibodies that could be targeting sperm.
- Sperm penetration assay (SPA): This analysis confirms that sperm have the ability to fertilize eggs.
- Ultrasound: This can detect varicoceles or duct obstructions in the prostate, scrotum, seminal vesicles, and ejaculatory ducts.
- Testicular biopsy: This can find whether sperm production is impaired or a blockage exists.
- Vasography: This is the best way to examine the duct system and any potential obstructions.
- Genetic testing: This can be used to rule out mutations of the Y chromosome as well as to test for cystic fibrosis.
After these evaluations have been completed, the next step is to develop a treatment plan.
How to Treat Male Infertility
The good news is that a variety of options exist for treating infertility in men. The specifics of infertility treatment vary depending on the underlying disease and the extent to which it impairs male fertility.
If the underlying cause can be categorized as pre-testicular, it can most likely be addressed by medical means. It's also possible to use surgery to address post-testicular infertility caused by obstruction.
Typically, doctors offer three types of treatment based on the patient’s specific issue: surgical treatment, non-surgical treatment, and treatment for unknown causes.
For patients with varicoceles, surgery may be required to correct the problem. A simple outpatient procedure, varicocelectomy involves repairing swollen veins to improve the movement, number, and structure of sperm.
Non-surgical treatments vary based on the specific condition and may include antibiotics to treat infections, medication to control erectile dysfunction or premature ejaculation, hormone replacement therapy, and counseling.
When it comes to testicular-based male infertility, treatment can be more complex. Often, the conception process will require using ART (assisted reproductive technology). These procedures involve obtaining sperm and inserting it into the female genital tract. Some methods of doing so include intrauterine insemination (IUI), in vitro fertilization (IVF), or IVF with intracytoplasmic sperm injection (ICSI). That last technique, IVF-ICSI, can result in pregnancy if even a few healthy sperm exist since it involves using a tiny needle to inject a single sperm directly into an egg.
Tips to Naturally Increase Fertility
In some cases, it can be possible to resolve more mild infertility issues using lifestyle changes and natural treatments. These steps can also complement other infertility treatments and boost overall health.
One of the best ways to protect long-term wellness is to be cognizant of chemical exposure. According to an article in GQ, environmental pollution can affect the shape of the sperm’s head and tail.
Men can boost their fertility by limiting alcohol consumption and avoiding cigarettes. Even reducing the number of cigarettes you’re smoking each day can make a difference in your health and fertility.
While regular exercise is a crucial part of staying fit, engaging in overly intense exercise routines can actually reduce sperm count. For best results, aim to work out at least 3 times a week and get plenty of rest in between. Amino Co's Athletic Performance blend can help increase performance gains and accelerate recovery between workouts.
Men who are concerned about fertility should also avoid wearing tight clothing, as overheating the testes can cause problems.
Finally, it’s important to sleep for a minimum of 7 hours a night to stay healthy and maximize your chances of conception.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















