Is It COVID? Watch Out for These Underlying Coronavirus Symptoms
 By: by Amino Science
By: by Amino Science
As national and worldwide health institutes get to know the coronavirus better the list of symptoms grows longer. Common markers of respiratory illness—cough, fever, shortness of breath—are now joined by a full gamut of ill effects—gastrointestinal distress, skin rashes, chest pain, congestion, loss of taste and smell, and more. Let’s get up to speed on underlying coronavirus symptoms so we know what to watch for as we safeguard our health.
Dominant Symptoms of COVID-19
There have been approximately 3.4 million reported cases of coronavirus disease in the United States since January 2020, when coronavirus was first detected, through mid-July 2020. Using data collected from symptom profiles of patients with laboratory-confirmed COVID-19, the Centers for Disease Control and Prevention (CDC) released a report July 17th that expanded the list of possible symptoms (1).
“Among 164 symptomatic COVID-19 patients, nearly all experienced fever, cough, or shortness of breath,” the CDC reported. “However, a wide variety of other symptoms were also reported; chills, myalgia [muscle soreness], headache, fatigue, and the presence of at least one [gastrointestinal] symptom (most commonly diarrhea) were each reported by >50% of patients.”
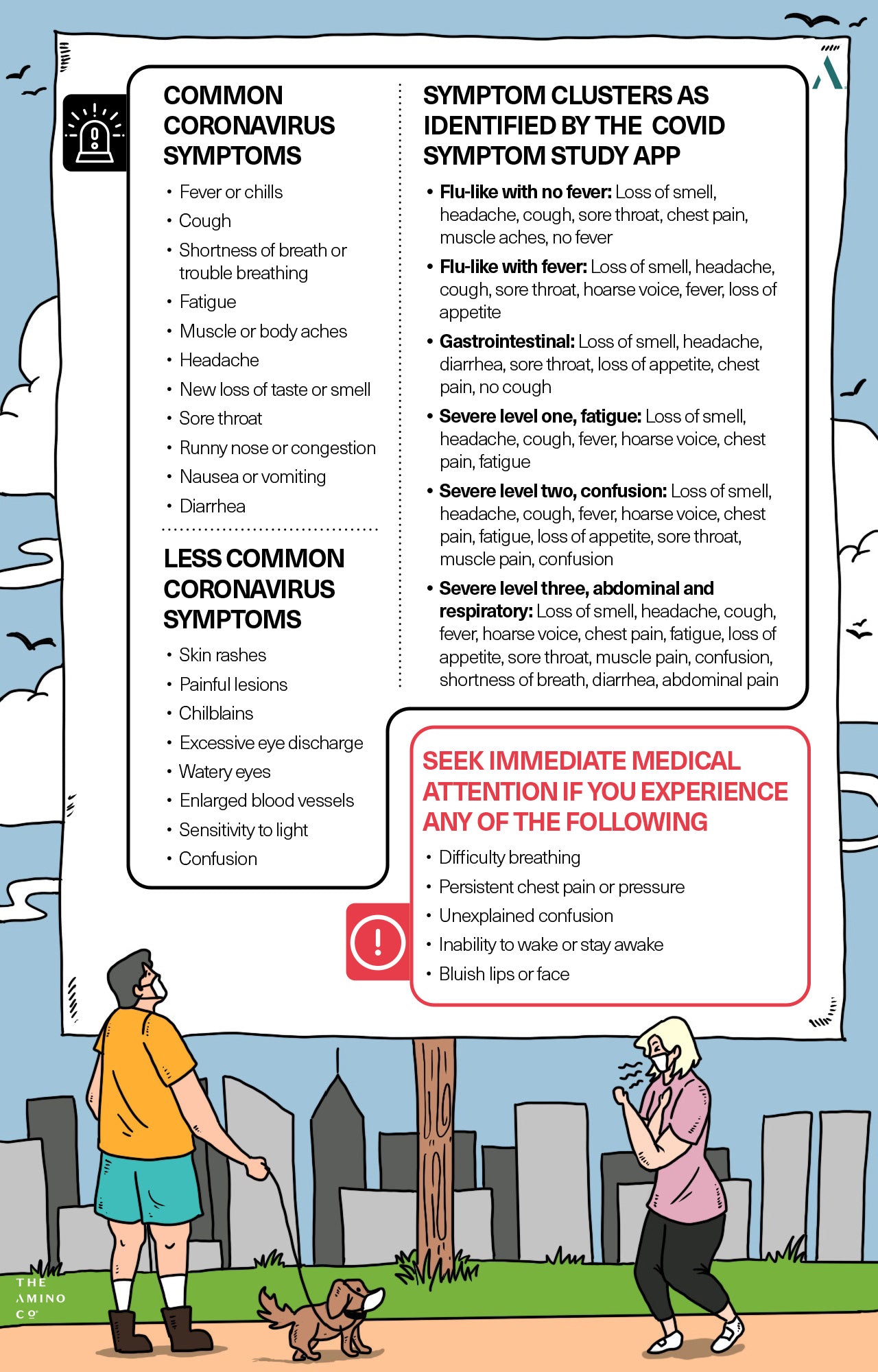
Using this data as a guideline, along with data from the World Health Organization (WHO), the CDC has expanded its list of common coronavirus symptoms to include:
- Fever or chills
- Cough
- Shortness of breath or trouble breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Runny nose or congestion
- Nausea or vomiting
- Diarrhea
The CDC acknowledges that the list is incomplete. To get a more comprehensive picture of underlying coronavirus symptoms, we can look to the COVID Symptom Study App developed by doctors and scientists at Massachusetts General Hospital, the Harvard T.H. Chan School of Public Health, King's College London, and Stanford University School of Medicine (2).
Underlying Coronavirus Symptoms
With more than 4 million users in America alone, the COVID Symptom Study App makes it easy for people to self-report symptoms and for researchers to track the data and identify new signs and developing hot spots of the virus. Because the app is available to the public, it also tracks nonhospitalized patients and mild symptoms that have previously gone underreported.
Andrew Chan, professor of immunology and infectious disease at the Harvard T.H. Chan School of Public Health and co-founder of the digital app explains, “The symptom that appears to be the strongest predictor of Covid continues to be a loss of taste or smell, and that’s been a thing that’s been continually shown in the data we’re getting in the app,” said Chan. “In particular, the fact that that symptom is relatively uncommon in other viral syndromes, certainly uncommon in seasonal allergies, makes it useful.”
That symptom has been included in the CDC’s list above, but other less common symptoms are emerging, including skin rashes, painful lesions, itchy, red skin, or inflammation on the fingers and toes. There have also been reports of chilblains, called COVID toes, that cause the hands and feet to swell and blister, although the jury’s still out as to whether that’s a COVID-related condition or more likely due to inappropriate footwear or sedentary behavior.
There have also been cases of COVID-19 linked to eye conditions, including swollen eyelids, watering eyes, excessive eye discharge, enlarged blood vessels, irritation, and a sensitivity to light, although these accounts have been attributed to more severe reactions to the virus. Severe infections in older people have also been linked to an increased likelihood of new confusion.
Taking into account these additional reports we can add the following to our coronavirus symptoms list:
- Skin rashes
- Painful lesions
- Chilblains
- Excessive eye discharge
- Watery eyes
- Enlarged blood vessels
- Sensitivity to light
- Confusion
COVID-19 Symptoms Aren’t Singular
SARS-CoV-2 doesn’t limit its effects to the respiratory system, which means symptoms aren’t solitary but can exist in clusters. Identifying those clusters may be key to catching COVID early, especially because so many symptoms overlap with symptoms of other viruses, such as the flu and the common cold.
The COVID Symptom Study App identified six symptom clusters from COVID-19 (3):
- Flu-like with no fever: Loss of smell, headache, cough, sore throat, chest pain, muscle aches, no fever
- Flu-like with fever: Loss of smell, headache, cough, sore throat, hoarse voice, fever, loss of appetite
- Gastrointestinal: Loss of smell, headache, diarrhea, sore throat, loss of appetite, chest pain, no cough
- Severe level one, fatigue: Loss of smell, headache, cough, fever, hoarse voice, chest pain, fatigue
- Severe level two, confusion: Loss of smell, headache, cough, fever, hoarse voice, chest pain, fatigue, loss of appetite, sore throat, muscle pain, confusion
- Severe level three, abdominal and respiratory: Loss of smell, headache, cough, fever, hoarse voice, chest pain, fatigue, loss of appetite, sore throat, muscle pain, confusion, shortness of breath, diarrhea, abdominal pain
Using these clusters, researchers were able to determine which symptom groups were more likely to require breathing support from ventilation or additional oxygen, as well as risk of hospitalization.
Individuals demonstrating symptom clusters 4, 5, and 6 with more severe symptoms are at higher risk of needing breathing support, and also tend to be older, overweight, or have a preexisting medical condition.
Lead researcher Dr Carole Sudre said: “Our study illustrates the importance of monitoring symptoms over time to make our predictions about individual risk and outcomes more sophisticated and accurate. This approach is helping us to understand the unfolding story of this disease in each patient so they can get the best care.”
When to Seek Immediate Medical Care
If you experience any of the following symptoms, seek immediate medical attention from urgent care or the emergency room, or call 911:
- Difficulty breathing
- Persistent chest pain or pressure
- Unexplained confusion
- Inability to wake or stay awake
- Bluish lips or face
Underlying Medical Conditions That Put You at High Risk of Severe COVID-19
No one is immune to Covid-19 infection, but those with underlying health conditions have been shown to fare the worst. According to a report released by the CDC in June 2020, individuals with preexisting conditions infected with COVID during the first 4 months of the pandemic were 6 times more likely to be hospitalized and 12 times more likely to die from the disease and its associated complications (4).
In addition to older adults and pregnant women, high risk individuals include people with:
- Heart disease
- Type 1 diabetes
- Type 2 diabetes
- Obesity
- Chronic kidney disease
- Weakened immune system
- Sickle cell disease
- Liver disease
- Lung disease
- Asthma
- Brain and immune system conditions
- High blood pressure
As the coronavirus attacks the body, a slew of complications can develop in both healthy individuals and those with the aforementioned health conditions:
- Pneumonia
- Respiratory failure
- Fluid in the legs
- Heart attack
- Stroke
- Organ failure
- Inflammation in the heart, muscle tissue, brain
- Sepsis
- Secondary bacterial infections
- Blood clots
- Multisystem inflammatory syndrome (in children)
If you are managing a chronic health condition, contact your health care provider so you can work together to reduce your risk of falling prey to serious illness.
Stopping the Spread of Covid-19
As the world works to eradicate the COVID-19 pandemic that’s traversed land and sea, several safety precautions have been proven effective. You can keep yourself and others safe from the new coronavirus by:
- Practicing social distancing (avoiding close contact and leaving 6 feet between you and others)
- Wearing a CDC-approved cloth face mask or other face coverings in public places
- Hand washing and using hand sanitizer frequently
- Keeping your immune system strong
Strengthening Immunity with Amino Acids
Amino acids play an important role in immune system function. They help activate T lymphocytes, B lymphocytes, natural killer cells, and macrophages. They regulate gene expression and lymphocyte proliferation. They help produce cytokines, antibodies, and other cytotoxic agents.
When disease strikes, such as coronavirus, immune system cells need extra energy...and fast! Taking a balanced formula of essential amino acids has been proven to increase mitochondria—the engines of the cells that drive all cellular functions, including eradicating viral and infectious agents. Amino acids also improve mitochondrial performance by increasing the number of enzymes involved in energy production.
If there aren’t enough essential amino acids to get the job done, then your immune system cells falter, leaving you more vulnerable to pathogens and disease. In times when your immune system needs to be operating on all cylinders, you can give it a hand by making sure you’re providing it with all the essential amino acids.
Amino Co formulas are designed to help improve immune function, reduce inflammation, and strengthen heart, kidney, and liver health. To learn more about our essential amino acids and how they target your most pressing health needs, shop our products here.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes





 833-264-6620
833-264-6620



















