What Is Bacterial Vaginosis: Symptoms, Causes, Treatments
 By: by Amino Science
By: by Amino Science

Bacterial vaginosis (BV) is the most common vaginal complaint in women of childbearing age, between 15 and 44 years old. While women in their reproductive years are most likely to get BV, it can affect women of any age. According to the Centers for Disease Control and Prevention (CDC) approximately 29% of women in the United States have BV.
Bacterial vaginosis is a vaginal infection that occurs when an overgrowth of bacteria upsets the delicate balance of bacteria in the vagina and triggers vaginal inflammation. About a quarter of pregnant women and more than half of women with an STD will at some point in time battle bacterial vaginosis.
What Is Bacterial Vaginosis?
Although it is not a sexually transmitted disease (STD) or a yeast infection, the symptoms of BV can mimic those found in vaginal yeast infections and sexually transmitted infections such as trichomoniasis. While the condition is usually not dangerous, Mayo Clinic physicians recommend seeking the consult of a gynecologist or nurse practitioner if you are experiencing atypical vaginal discharge to rule out serious infections such as gonorrhea and chlamydia.
BV Causes
Certain activities, such as unprotected sex or frequent douching (which pushes bacteria farther into the genital tract), are thought to increase the risk of bacterial vaginosis infection. BV rarely occurs in people who have not had sexual intercourse, and can commonly occur after having sex with a new partner or when having multiple sex partners, although the role of sexual activity in the development of the condition is not fully understood.
Other risk factors include:
- Using water or a medicated solution to clean the vagina
- Bathing with antiseptic products
- Using scented personal hygiene products
- Smoking
- Using IUDs (intrauterine devices) for birth control
- Taking antibiotics recently
- Cleaning underwear with powerful detergents

The Bacteria in Bacterial Vaginosis
The vagina contains different types of bacteria, or vaginal flora. Lactobacilli bacteria produce lactic acid, rendering the vagina somewhat acidic and keeping other bacteria from growing there. Reduced lactobacilli levels lower the vagina’s acidity, giving harmful bacteria the opportunity to multiply.
BV is not a true bacterial infection. Instead, it occurs when there are a disproportionate number of the usual vaginal bacteria. It is not considered a true infection in which there are foreign bacteria, as is the case with numerous sexually transmitted diseases.
Often referred to as nonspecific vaginitis, BV was formerly called Gardnerella vaginitis. It was named for the bacteria suspected of being responsible for the condition, Gardnerella vaginalis. Bacterial vaginosis, the current moniker, reflects the concept that more than one kind of bacteria can be present in the vagina and can overproduce.
Bacterial vaginosis entails a variety of bacteria besides Gardnerella that fuse together—Bacteroides, Eubacterium, Lactobacillus, Fusobacterium, and Peptostreptococcus, to name a few. For unknown reasons, these bacteria join forces to create an imbalance in the vagina. Although the number of lactobacilli that produce hydrogen peroxide may be lowered, there may be a higher intensity of anaerobic bacteria that grow when oxygen is lacking, as well as other kinds of bacteria. Because so many possible combinations exist, it is difficult to diagnose and treat BV.
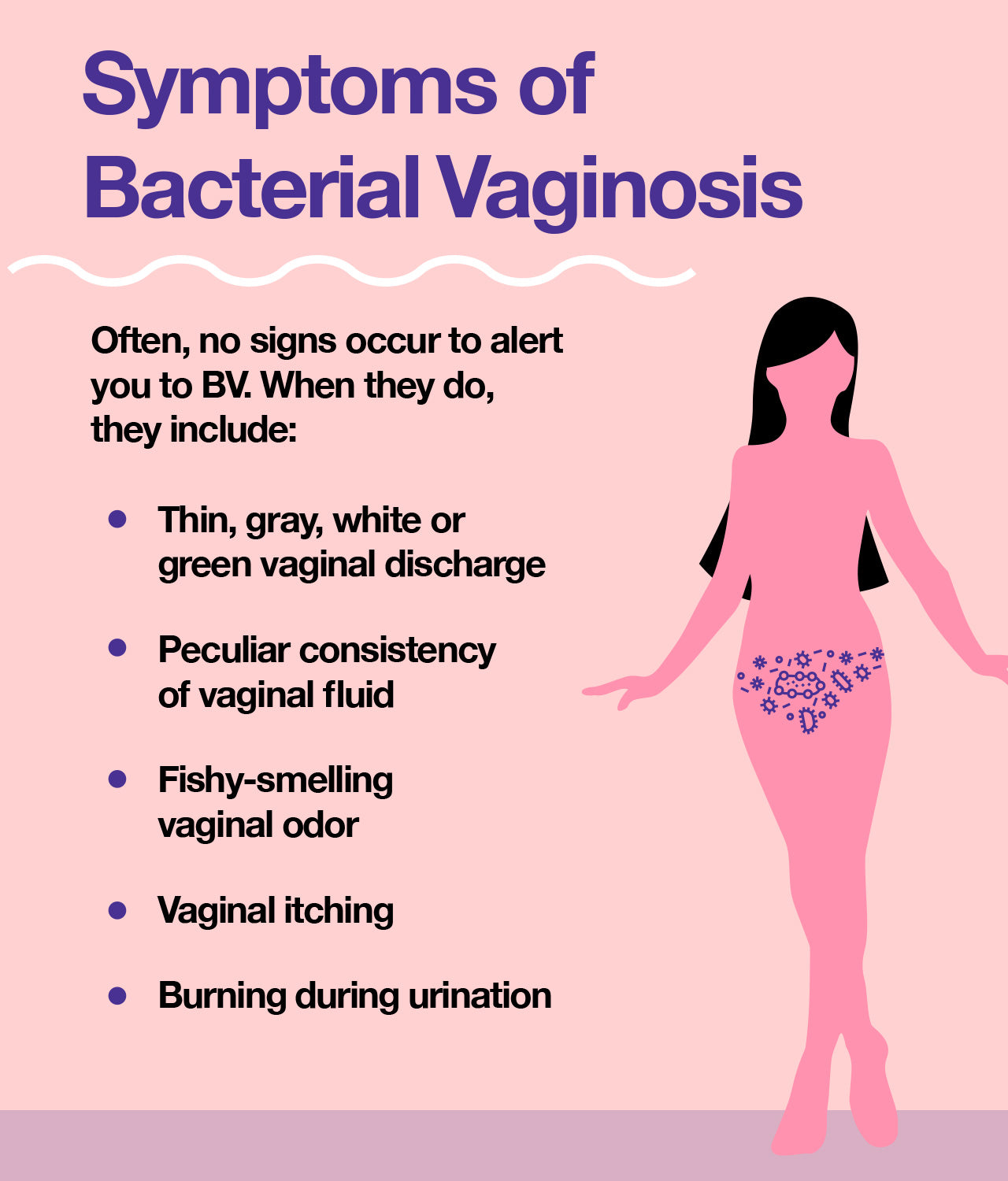
BV Symptoms
Between half and three-quarters of women with BV do not have symptoms. Vaginal discharge with the following symptoms may be caused by BV or a variety of other complications, such as a yeast infection, STD, and menopause.
- Thin, green, white, or gray discharge from the vagina
- Peculiar consistency of vaginal fluid
- Odorous fishy smell emanating from the vagina
- Itching in the vaginal area
- Burning sensation when urinating
Symptoms of BV in women can present at anytime during the menstrual cycle. Normal amounts of discharge vary from woman to woman, and what is considered abnormal for one, may not be for another, which is why regular attention to your vaginal health and an annual visit to a gynecologist is recommended.
BV Complications
While BV is not considered an STI, it increases the risk of developing an STI.
Complications linked to BV entail a higher risk of:
- HIV infection (because BV makes people more susceptible to the virus)
- STIs (including human papilloma, herpes simplex, gonorrhea, and chlamydia)
- Infection that develops after a procedure such as an abortion or a hysterectomy
- Potential complications of BV during pregnancy are:
- Preterm delivery
- Termination of pregnancy
- Early opening of the amniotic sac
- Postpartum endometritis
- Tubal factor infertility
BV during pregnancy can also put you at risk for chorioamnionitis, an inflammation of the membranes surrounding the fetus that increases the chance of early delivery. A newborn who survives this kind of delivery has a higher than normal risk of cerebral palsy.
Pregnant women are also more likely to have preterm births or babies with low birth weight. BV can also decrease the success rate of in-vitro fertilization (IVF) and increase the risk of pelvic inflammatory disease (PID), an infection of the fallopian tubes, uterus, and ovaries that can cause infertility.
About 30% of women successfully treated for BV will have a recurrence within three months, and 50% will have a recurrence within six months. If symptoms of BV persist or recur, or you are pregnant it's imperative to visit your health care provider for further testing. If symptoms disappear after finishing a course of antibiotics, it's not necessary to test for BV again.
When to See a Doctor
The Mayo Clinic recommends seeing a doctor when new vaginal discharge accompanies a fever or unusual smell, the color and texture of the discharge appears different from that of previous infections, there is more than one sexual partner or a new one, or symptoms persist after using a non-prescription treatment for a yeast infection. While BV can resolve without treatment, it's best to seek medical advice to avoid complications. Seeing a doctor quickly can rule out other infections, such as gonorrhea or trich.
BV Diagnosis
When a woman becomes aware of an unusual vaginal discharge and tells her doctor about it, the doctor will ask questions that help to determine whether she has BV or more serious conditions, perform a pelvic exam, do a visual inspection, and test for chlamydia or gonorrhea.
Diagnostic tests use a swab or small plastic loop to collect sample cells from the vaginal wall and measure the pH balance of the vagina to determine acidity levels. BV in women can be determined by a low lactobacilli bacterial count and a vaginal pH greater than 4.5.
A look under the microscope can reveal clue cells, which are bacteria-covered vaginal cells that indicate a bacterial vaginosis infection is present. Your doctor will often perform a “whiff test” using potassium hydroxide (KOH) liquid to determine if you are indeed besieged by the fishy odor associated with BV.
BV Treatment
About one-third of BV cases are said to resolve on their own, but medical treatment is recommended to avoid complications. BV is normally treated with antibiotics, which work in as many as 90% of cases, but BV can recur within a month.
The most frequent antibiotic prescribed is Metronidazole. It is available as tablets taken orally, twice a day for 7 days; as a single tablet taken orally as a one-time dose; or as gel applied to the vagina once daily for 5 days. Metronidazole, which reacts with alcohol, can make the patient feel very ill if alcohol is consumed within 48 hours.
Clindamycin, another antibiotic, may be prescribed if metronidazole is not working or if the BV comes back. Pregnancy prevention aids, such as latex condoms, diaphragms, and caps, may not work well when you are on Clindamycin.
Another antibiotic, Tinidazole, is administered if metronidazole fails to work or if BV recurs. This medication is taken orally as a single dose, and it requires the avoidance of alcohol.
When symptoms recur, they may be addressed with a 7-day dosage of vaginal or oral antibiotics. If the first treatment was oral, bacterial vaginosis treatment could be more effective on the second attempt, and vice versa. If there are more than three occurrences within 12 months, the physician may give the patient a course of vaginal metronidazole gel to use vaginally 2 times a week for up to 6 months. Serious BV complications of bacterial vaginosis can happen during pregnancy, with recurrence possible even after successful treatment. Over half of the people who are treated for BV have the symptoms again in less than a year.
While there is no approved over-the-counter medication for BV, some researchers believe that probiotics can help to treat it without adverse effects.
One study compared the results of 1 week of oral metronidazole (500 milligrams) twice daily along with 30 days of oral probiotics versus the same dose and duration of metronidazole plus 30 days of placebo. After 1 month the recurrence rate was 12% in the antibiotic/probiotic group vs. 60% in the antibiotic/placebo group. This study demonstrates the efficacy of vaginal probiotic capsules to treat BV. Because the study was sponsored by the makers of the capsule, additional research is needed to determine whether other probiotic formulations, administered orally or at the site of the infection, are effective.
Preventing BV
A common women's health concern, BV is difficult to prevent but there are steps you can take to limit its occurrence. Steer clear of vaginal douches, keep the number of sex partners at a minimum or practice monogamy, and use BV medications as prescribed. If you suspect BV, visit your gynecologist or primary care physician to avoid complications and rebalance your vaginal flora. In the meantime, keep your immune system strong with essential amino acids.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes



 833-264-6620
833-264-6620



















