Causes, Signs and Treatment of Ischemic Colitis
 By: by Amino Science
By: by Amino Science

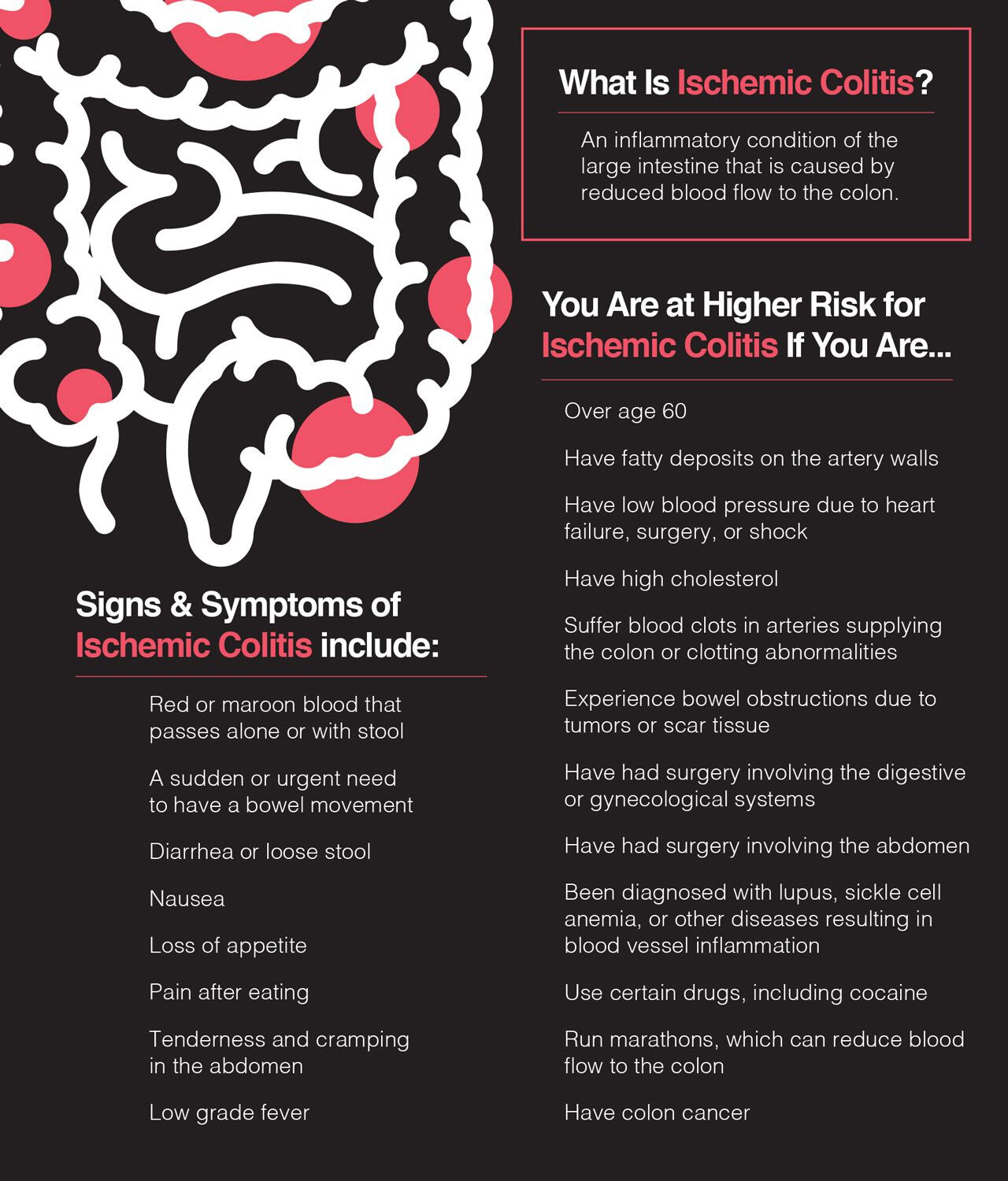
Ischemic colitis is a serious medical condition in which blood flow to part of the colon (large intestine) is reduced. This reduced blood supply results in intestinal ischemia, which can cause abdominal pain and bloody diarrhea.
Ischemic colitis is also sometimes confused with mesenteric ischemia. Though both conditions occur within the distribution of the mesenteric artery, mesenteric ischemia is a much more serious and sometimes life-threatening condition that affects the small bowel.
Of the several types of ischemia affecting the gastrointestinal (GI) tract, ischemic colitis is the most common and accounts for 1 in 2,000 hospital admissions.
In this article, we’re going to examine the most common causes of ischemic colitis, symptoms associated with the condition, and types of management used to treat this often frightening and painful condition.
Understanding What Causes Ischemic Colitis
Ischemic colitis can be caused by a variety of conditions, both occlusive and nonocclusive. Nonocclusive ischemia is the result of low blood pressure or constriction of the vessels feeding the colon. Occlusive ischemia occurs when a blood clot or other impediment blocks blood flow to the colon.
However, the biggest risk factor is age, with the majority of cases being seen in people over 60. It’s also more commonly seen in people with heart and blood vessel disease and clotting disorders.
In addition, ischemic colitis can be the result of colonic ischemia due to abdominal surgery, strenuous exercise (such as that engaged in by endurance athletes), cocaine and methamphetamine use, and certain medications, including nonsteroidal anti-inflammatory drugs (NSAIDs), antihypertensives, and birth control and migraine medications.
Additional occlusive conditions that can lead to ischemic colitis include:
Additional nonocclusive conditions that can lead to ischemic colitis include:
- Chronic constipation
- Low blood pressure
- Colon cancer
- Heart failure
- Blood clots
Signs and Symptoms of Ischemic Colitis
The first sign of ischemic colitis is generally sudden onset of mild to moderate abdominal pain and cramping. While pain is often felt on the left side, it can be felt anywhere in the abdomen and may be accompanied by an overwhelming urge to defecate.
In cases involving the right side of the abdomen, stool may be mixed with dark red clots, while cases involving the left side may present with the passage of bright red blood in the absence of stool. Additional symptoms may include:
- Abdominal tenderness
- Diarrhea
- Nausea
- Loss of appetite
- Pain after eating
- Low-grade fever
While most cases of ischemic colitis generally resolve without complications within one to two weeks, in severe cases, ischemic colitis can result in damage to the colon, including gangrene of the affected region and intestinal perforation.
These risks are even greater if symptoms present on the right side of the abdomen, for not only can symptoms on this side be more severe, but they can also indicate that blood flow to the small intestine has been compromised.
If this occurs, the risk of intestinal tissue death is even more significant, and surgery is required to prevent life-threatening complications.
Because early diagnosis and treatment are the best way to prevent serious complications, it’s recommended that you seek medical treatment as soon as possible if you experience sudden, severe abdominal pain or bloody diarrhea.

Diagnosing Ischemic Colitis
Since the signs and symptoms of ischemic colitis often overlap with other conditions—especially inflammatory bowel disease—your health care provider will probably decide to conduct additional tests after performing the initial physical exam.
However, diagnostic tests such as laboratory studies and x-rays are generally not helpful in diagnosing ischemic colitis, so other studies will likely be performed. The most common of these are:
- Computed tomography (CT scan)
- Ultrasound
- Colonoscopy
After testing has ruled out other disorders—such as infections, inflammatory bowel disease, and acute mesenteric ischemia—and confirmed the diagnosis of ischemic colitis, treatment will then depend on the severity of your condition.
Ischemic Colitis Treatment Options
Ischemic colitis is a serious medical condition for which hospitalization is required.
Patients with no signs of nonviable bowel on colonoscopy or symptoms of peritonitis (inflammation of the peritoneum, the membrane lining the abdominal cavity and organs)—a medical emergency—can be managed without surgery. Symptoms of peritonitis include:
- Severe abdominal pain
- Abdominal tenderness
- Abdominal guarding
Medical management of ischemic colitis is focused on allowing the intestine time to rest by placing the patient on intravenous (IV) fluids and protecting them from secondary infections via the use of broad-spectrum antibiotics.
If the cause of the ischemic colitis is determined to be something that can be eliminated, such as a medication, then that factor will be removed as well.
Patients with underlying heart or lung conditions, such as congestive heart failure (CHF) and chronic obstructive pulmonary disease (COPD), will also receive treatment to optimize cardiac function and oxygenation.
With appropriate medical management, the majority of patients improve within 24 to 48 hours. However, approximately 20% of people fail to show improvement during this time frame and may exhibit signs of a perforated bowel, uncontrolled bleeding, or peritonitis.
If any of these complications is noted, it’s a sign of a medical emergency, and surgery must be performed.
Surgery for Ischemic Colitis
Surgical treatment for ischemic colitis will depend on the stability of the patient’s condition and the type and extent of damage the bowel has sustained. For example, surgery may be needed to:
- Remove scar tissue causing bowel obstruction
- Repair a perforation
- Remove dead tissue
- Bypass a blocked artery
While patients requiring surgery for ischemic colitis have the highest rates of complication and death, those with right-sided involvement have the highest mortality rate.
To improve recovery outcomes, supplement with the surgical recovery blend Heal, clinically proven to help you recover faster, maintain muscle mass during bedrest, and increase physical strength and function as soon as 6 weeks after surgery.
After Ischemic Colitis: Recovery and Prevention
When your symptoms have subsided, your health care provider may recommend a clear liquid diet to help ease your colon back into the business of processing nutrients.
The next step in your recovery may be what’s known as a low-residue diet. This type of diet limits fiber-rich foods, with the goal of fewer, smaller bowel movements. Low-residue foods include:
- White bread and rice
- Cooked cereals
- Skinned and seeded cooked vegetables
- Tender meats and poultry
- Dairy products
- Eggs
- Bananas
- Cantaloupes
- Avocados
Unfortunately, beyond the implementation of dietary changes during recovery from a bout of ischemic colitis and follow-up colonoscopy to assess response to treatment, there’s no surefire approach to preventing future recurrences.
As we’ve seen, ischemic colitis can be caused by a variety of factors, and many times the cause is never determined. Most people with ischemic colitis also tend to recover quickly and may never experience another episode.
Therefore, the wisest course of action may simply be ensuring the optimization of treatment for medical conditions known to contribute to ischemic colitis and eliminating any medications that may lead to the condition.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















