Cellulitis Skin Infection: What Causes It and How Do You Treat It?
 By: by Amino Science
By: by Amino Science

Everyone gets the occasional dry skin, heat rash, or unexplained red patch on their skin from time to time. Too much sun, intense heat, and allergic reactions to plants, animals, or household items like laundry detergent are all common causes of skin irritation. However, if a rash doesn’t clear up after a day or two, seems to be expanding, or is accompanied by fever or warm, swollen skin, it could be more than just a rash. When a rash presents with symptoms like these, it’s time to seek medical advice to rule out infections like cellulitis.
What Is Cellulitis?
Cellulitis is a common bacterial infection that affects the thick middle layer (dermis) and innermost layer (subcutaneous tissue) of the skin. According to the American Academy of Dermatology (AAD), approximately 14.5 million cases of cellulitis are diagnosed in the United States each year.
Causes of Cellulitis
Most cases of cellulitis are caused by two types of bacteria: Streptococcus (strep) and Staphylococcus (staph). However, the more serious methicillin-resistant Staphylococcus aureus (MRSA) is becoming an increasingly common cause of both skin and soft tissue infections and is now estimated to comprise approximately 25% of cases of cellulitis.
While cellulitis can appear anywhere on the body, in adults, it most commonly affects the skin on the lower legs. However, in children, the face and neck are the sites most frequently involved.
Whether the infection concerns children or adults, the bacteria that cause cellulitis are most likely to enter the skin through injuries such as cuts, surgical and puncture wounds, burns, and ulcers. Skin disorders that result in cracking or flaking, such as athlete’s foot, eczema, and dermatitis, can also allow bacteria to enter the body.
In healthy people with normal immune system responses, these infection-causing bacteria are destroyed before they have a chance to cause problems. However, in people with certain illnesses or compromised immune systems, bacteria may enter even dry or swollen areas of skin, where they then proliferate and lead to infection.
Symptoms of Cellulitis
The symptoms of cellulitis may spread rapidly but usually begin with redness and swelling. As symptoms progress, you may also notice the following signs of infection:
- Warmth
- Tenderness
- Red spots
- Blisters
- Skin dimpling
- Fever
Risk Factors for Cellulitis
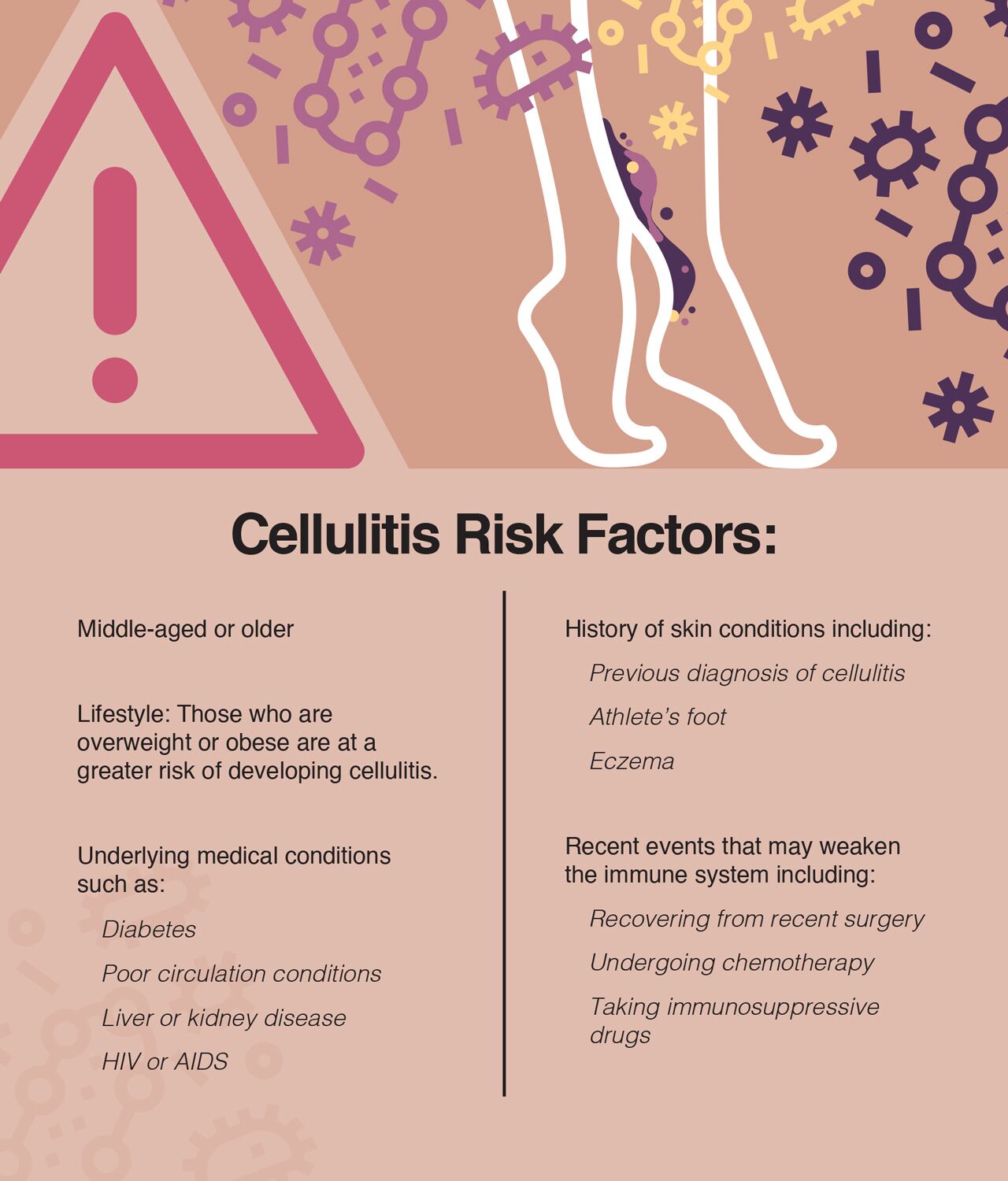
Even though anyone can develop cellulitis, certain groups do have a greater chance of having the condition. Among these are people with:
- Weakened immune systems: Those with conditions such as diabetes, cancer, or human immunodeficiency virus (HIV) are more prone to develop cellulitis.
- Lymphedema: Chronic swelling, which sometimes occurs following surgery and usually affects the arms or legs, can increase your risk.
- Skin disorders: Those with skin conditions that cause breaks in the skin, such as eczema and athlete’s foot, are at greater risk.
- History of cellulitis: Those who’ve had cellulitis in the past have a greater risk of developing it again.
- Frequent skin injuries: Residents of nursing homes, prisoners, athletes, and intravenous drug users are all at greater risk.
- Obesity: People who are obese tend to also suffer from related medical conditions, such as leg swelling, diabetes, poor circulation, and retained moisture in body folds, all of which can lead to infection of the skin and cellulitis.

Diagnosing Cellulitis
While your health care provider will most likely be able to diagnose cellulitis by performing a simple physical exam of your skin, the Infectious Disease Society of America (IDSA) recommends that patients who are immunocompromised, exhibit systemic toxicity (sepsis), or have sustained animal bites undergo additional tests, including blood cultures, to help guide treatment.
Treatment for Cellulitis
Once diagnosed, prompt treatment is essential to prevent the bacterial infection from spreading to other parts of the body, such as the bloodstream or lymph nodes. Spread of the infection to either of these locations can quickly become life-threatening.
Recurrent episodes of cellulitis may also damage the lymphatic system and lead to chronic lymphedema of the affected extremity, and infection that enters the bloodstream can lead to sepsis.
In rare cases, the infection may spread to the connective tissue beneath the skin (fascia) and result in necrotizing fasciitis—commonly known as flesh-eating disease—a severe complication that spreads rapidly and can result in death.
However, as long as cellulitis is caught early and treated appropriately, the condition generally clears quickly, without complications.
The therapy most commonly used to treat this bacterial skin infection includes:
- Oral antibiotics: Oral antibiotics may be prescribed for 5 to 14 days, but symptoms of cellulitis should begin to improve within 24 to 48 hours. However, in severe cases where the cellulitis doesn’t respond to oral antibiotics or extensive symptoms and high fever are present, hospitalization and intravenous antibiotics may be necessary.
- Elevation: If possible, the part of the body affected by the cellulitis should be elevated above the level of the heart to help reduce swelling and speed recovery.
- Keeping the area clean and dry: The infected area should be kept clean and dry. A dressing may also be applied for protection. However, antibiotic ointments and creams should not be used.
Preventing Recurrence
Because people who’ve had cellulitis have a higher risk of recurrence—usually in the same location—certain steps are recommended to help keep the infection from coming back. These include:
- Avoiding skin injuries: Preventative measures such as always wearing shoes and keeping nails trimmed to prevent scratching can help reduce your risk of recurrent cellulitis.
- Taking care of new wounds: Inspecting skin for signs of injury and washing open wounds, applying over-the-counter antibiotic ointment, and covering with a bandage daily can reduce risk of recurrence.
- Cleaning and moisturizing: Keeping the skin clean helps remove bacteria, and moisturizing regularly helps keep skin moist and free of the cracks that allow bacteria to enter.
- Treating superficial infections early: Treating superficial skin infections such as athlete’s foot and impetigo at the first sign can help prevent their spread and reduce cellulitis risk.
- Treating related medical conditions: Getting conditions known to increase the risk of cellulitis—including diabetes, peripheral artery disease, and lymphedema—under control can reduce your chance of developing the condition.
- Losing weight: Studies show that obese people who lose weight decrease their risk of recurrent episodes of cellulitis. For help with weight loss and boosting your immune system, check out our premium amino acid supplements.

When a rash isn’t just a rash, it can be a scary thing. And left untreated, cellulitis can quickly become a life-threatening condition. But when it’s caught early, cellulitis treatment is usually quick and relatively easy.
So if you discover a rash that’s red, swollen, tender, warm, and expanding, don’t wait. See your doctor right away. After all, the sooner you get started, the easier it will be and the faster you can get back to living your life.

Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















