Nutrition for the Gut: What You Need to Know to Achieve Healthy Gut Function
 By: by Amino Science
By: by Amino Science

"The burden of digestive diseases in numerical terms remains staggering in the United States," states a report issued by the National Institutes of Health (NIH). Estimates indicate that 70 million individuals in the United States have been diagnosed with a digestive illness (excluding heartburn) and that these malfunctions of the digestive system account for close to 10% of total health care spending each year. Understanding optimal nutrition for the gut is key to both preventing and treating the rampant digestive issues afflicting the population.
We are just beginning to understand the multitude of ways in which the gut microbiome impacts not just gut health but overall immune function and systemic health. Almost 70% of our immune system cells live in or around the gut. Beneficial gut bacteria not only ensure that we fully digest the food we eat and enhance the absorption of minerals, but they also help manufacture vitamins (specifically, vitamins B3, B5, B6, B12, and K as well as folate and biotin) and fight off pathogens.
Anyone who has suffered gastrointestinal distress can appreciate how vital an intact, healthy gut is to our overall health.
To fuel optimal gut function, you must offer your body a steady supply of key nutrients. Glutamine ranks high on the list thanks to its ability to support the transit of nutrients into the blood and the replenishment of cells damaged in the line of duty.
Understanding Ideal Nutrition for the Gut
Not only does your gut break down the foods you consume so that your body can absorb the nutrients it contains, but it also acts as a selectively permeable barrier between the body and foreign particles we ingest (intentionally or unintentionally).
When we eat to satisfy hunger, we fill our stomach with nutrients to meet the body’s demand for energy and with micronutrients for all the chemical reactions that keep organs and muscles functioning throughout the body. A significant number of these compounds are put to use right away to keep the gut healthy and intact.
We often talk about nutrition and nutrients in a general sense, but specific nutrients fulfill precise roles within the human body. For instance, amino acids support muscle growth. Your body also requires certain nutrients to maintain proper gut function.
When the gut does not receive those nutrients, it enters a state of distress in which it can no longer carry out its digestive or protective roles. This can lead to irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), leaky gut, celiac disease, food sensitivities, bacterial imbalances, or overlapping diagnoses of various digestive disorders.
What Healthy Gut Function Looks Like
The gut is not just a passive structure through which food passes to be digested and absorbed. Instead, it is a dynamic and complex microenvironment that harbors many organisms and cells working in concert to process nutrients for absorption and waste products for excretion.
As mentioned above, the gut acts as a barrier between your body and the outside world. Its lining—the gut mucosa—serves not only as a protective barrier but also as a key player in immune function and nutrient metabolism.
Epithelial cells line the gut mucosa, establishing a barrier between the external environment and the internal mixture of nutrients and digestive materials. The barrier is selectively permeable to allow for the passage of nutrients outward to the periphery and waste products inward for excretion.
The cells in the gut must be able to grow and replace themselves quickly because they are exposed to a constant stream of nutrients, digestive factors, toxins, and pathogens that pass through. In fact, it is estimated that every person processes almost 60 tons of food in a lifetime!
As it divides, integrates, and eliminates the subcomponents of all that food, as well as proteases, microbes, alcohol and drugs, and other substances, the gut mucosa sustains ongoing damage. It must regenerate healthy new cells to maintain the integrity of the barrier.
In addition to its regenerative capacity, a healthy gut barrier requires a proper balance of intestinal bacteria as well as a fully functioning immune system.

How the Gut Delivers Nutrients to the Body
The gut uses two types of transport to convey the nutrients extracted from food to the cells that need them: passive and active.
Passive transport is simply diffusion of the substance from one space to another. Fats, water, and some minerals and B vitamins are examples of nutrients that move down a concentration gradient to be absorbed by passive diffusion.
Larger molecules like glucose and amino acids have to actively resist that same gradient, moving up it into a space that has a relatively higher concentration. This requires energy and a process called active transport.
The gut itself must take in a steady supply of certain nutrients—namely, glucose and the B vitamins involved in energy metabolism— to fuel active transport.
The Link Between the Gut Microbiome and Overall Human Health
The human body, like any other environment on the planet, has its own ecosystem. Research has shown that, on average, each human being harbors between 10 trillion and 100 trillion microorganisms, or microbes, including bacteria, fungi, viruses, and other single-celled organisms. A variety of estimates place the number of individual species of microbes found in the human body at approximately 1,000.
The term "human microbiome" refers to all the genes inside this vast variety of microbial cells, which outnumber our own bodies' genes by 100 to 1.
The gut contains the densest concentration of microbes, as well as the most diverse range of species, in the entire human body. Human gut microbiota live within a thin layer of mucus that lines the large intestine. The microbes residing there form a protective biofilm and also carry out a number of helpful tasks that support overall human health.
The composition of the human gut microbiota varies significantly from person to person depending on factors such as:
- Genes
- Age
- Diet
- Physical environment
Factors right down to your occupation can alter the composition of your microbiota. And your gut microbiome, in turn, can affect not only your utilization of nutrients and immune function, but also your mood, sleep, perception of pain, and stress levels.

1. Mood
Sometimes called "the second brain," scientists have discovered that the enteric nervous system in the gut holds 30 different neurotransmitters as well as 100 million neurons.
Research on the gut-brain axis has yielded valuable insight into how the health of your gut impacts mental health conditions such as depression and anxiety.
Consuming foods that positively impact the makeup of your gut microbiome can lead to improved mental health. According to a 2017 study, mice fed probiotic-rich yogurt experienced dramatic decreases to depression symptoms.
2. Sleep
Serotonin, one of the neurotransmitters produced in the gut, helps to produce melatonin which is known colloquially as the sleep hormone.
A study published in the World Journal of Gastroenterology documented the presence of 400 times more melatonin in the gut than exists in the brain.
3. Inflammation
Microbes found in the gut release compounds with potent anti-inflammatory properties. Maintaining appropriate levels of these microbes can prevent and combat inflammation throughout the body, thereby lowering your risk of developing a number of chronic diseases.
4. Immune Function
The microbes in the the human gut microbiota halt the development of harmful bacteria that can cause infections. The anti-inflammatory capacity of certain microbes also support healthy immune function.
5. Skin Wellness
Studies, including this article published in Nature Review Microbiology, have found that areas of the body with increased oil production, such as the back and the face, have decreased microbial diversity. This appears to be because oil acts in an antimicrobial fashion.
The microbes native to those areas of the body have the capacity to draw out the moisturizing properties of the oil present there, keeping the skin soft and supple. Well-moisturized skin also has enhanced defensive abilities that keep potentially deleterious bacteria from entering the body.
What Undermines Gut Health?
Human nutrition is, unquestionably, the risk factor for poor gut health over which we have the most control. However, no single dietary pattern has been identified as advantageous or disadvantageous for all individuals.
That said, researchers have found poor gut health can often be traced back to four food compounds: lectins, gluten, fructose, and dairy immunoglobulins.
- Lectins: A category of protein compounds. Those with the most damaging effect on human health come from seeds, nuts, grains, and beans and legumes.
- Prolamines: Another category of protein compound—most infamously, gluten—that exist naturally in grains. Other prolamines include hordein from barley, secalin from rye, and zein from corn.
- Fructose: In the simplest terms, fruit sugar. Individuals whose digestive systems are aggravated by fructose often find a category of complex carbohydrates known as fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) to be difficult to digest as well.
- Dairy immonoglobulins: This category of compounds includes lactose and casein.
These compounds produce poor gut health in various ways. The mildest occur when individuals lack the appropriate enzymes to digest one or more of the compounds. This results in symptoms like an upset stomach, gas, bloating, constipation, and/or diarrhea.
In other cases, they may stimulate mast cells to produce histamine. This response can mimic a food allergy, leading to increased intestinal permeability and systemic inflammation. Alternately, it can present like respiratory allergies, generating symptoms such as sneezing and congestion.
It's also possible for these food compounds to cause the immune system to release T-cells. Yet another potentiality is that they create or exacerbate autoimmune diseases.

Optimizing Nutrient Intake for a Healthy Gut
We have learned from situations in which people receive their nutrition by intravenous feeding (parenteral nutrition) that the gut thrives when able to run through all the elements of the digestive process. Like your muscles, it will atrophy if it is not exercised.
Dietary fiber is a very important part of this mechanical aspect of digestion and gut health. Fiber provides bulk to support healthy bowel movements and is an equally important source of fermentable fuel for the billions of healthy bacteria in our gut.
Fascinatingly enough, it seems that not only does the food we eat affect gut health, but also vice versa. The gut microbiome sends small molecules into the bloodstream, which impacts a multitude of functions, such as how the body stores nutrients and responds to sugar. These molecules also regulate our appetites and can even play a key role in weight-loss efforts.
Eating a Western diet high in processed foods can create a negative feedback loop. The more damaging foods you eat, the worse the health of your gut becomes. The worse the health of your gut, the more damaging foods you crave. This can produce increased gut mucosa permeability and inflammation, among other adverse effects.
But it's possible to help your gut heal by taking simple, actionable steps. Here are some suggestions for how you can optimize your nutrient intake to encourage gut health. Remember, as discussed in the previous section, no single nutritional approach can be universally applied. Finding the right strategy for keeping your population of gut microbes healthy and limiting the growth of bad bacteria will require some trial and error.

1. Diversify Your Diet
The wider the range of foods you eat, the more diverse your microbiome will become. Scientists have discovered a clear correlation between biome diversity and good health. Fiber-rich legumes, beans, and fruit foment the growth of a particularly beneficial kind of microbe, Bifidobacteria.
2. Weed Out Problematic Foods and Beverages
You can do this on your own by researching the protocol for elimination diets, but it can be helpful to seek guidance from a professional. If you intend to eliminate multiple food groups, professional help is especially advisable so you can avoid potential nutrient deficits.
3. Embrace Fermented Foods
Fermented foods like yogurt, sauerkraut, and kefir can have serious health benefits thanks to the healthy bacteria, known as probiotics, that they contain.
Experts say probiotics—notably, Lactobacilli—can cut down populations of microbes known to cause disease. Probiotic supplements are one way to benefit from these healthful compounds, but some believe it's even better to get them directly from whole food sources.
4. Give Prebiotic Foods Their Due
Probiotics have received the lion's share of attention, but prebiotics appear to be every bit as essential to gut health. This specialized type of fiber stimulates the growth of beneficial gut bacteria.
Look for prebiotic-rich foods like artichokes, bananas, asparagus, oats, and apples.
5. Avoid Artificial Sweeteners
Studies show that low- or no-calorie sweeteners like aspartame can cause massive damage to the health of your gut.
It seems that ingesting these sweeteners escalates the growth of a bacteria called Enterobacteriaceae that can cause unpleasant infections throughout the body.
The sugar alcohols used to sweeten many kinds of gum, protein powders, and sugar-free desserts can be altogether deleterious. They're common culprits behind symptoms like persistent bloating and stomach cramps.
6. Experiment with Whole Grains
Grains can produce digestive distress for some individuals, but they're certainly not an innately unhealthy food. Quite the opposite, in fact.
They're a key source of dietary fiber, particularly beta-glucan. Studies show that the health benefits of beta-glucan include improved weight management, decreased cancer risk, lowered odds of developing type 2 diabetes, and more.
7. Try a Plant-Based Diet
Plant foods seem to be uniquely beneficial for gut health.
Studies reveal adhering to a vegetarian diet can cause levels of health-damaging bacteria like E. coli to drop. Plant-based diets have also been shown to lower cholesterol and inflammation levels.
If you opt for a plant-based diet, be sure to supplement with essential amino acids to make sure you are meeting your protein needs.
8. Seek Out Polyphenols
When your gut absorbs these plant compounds, they invigorate the growth of friendly bacteria. You can find polyphenols in whole grains, olive oil, green tea, dark chocolate, and red wine.
9. Stay Away from Unnecessary Antibiotics
Antibiotics can be life-saving when taken appropriately. Some doctors can be convinced to prescribe antibiotics when they're not medically necessary, however. For example, to treat a viral infection.
Because antibiotics kill both bad and good bacteria indiscriminately (not to mention rising rates of antibiotic resistance), it's important to only take antibiotics when they are truly indicated as the best treatment approach.
10. Take Time to Chew Thoroughly
Your mother may have been on to something when she told you to slow down and take smaller bites.
Scientists have ascertained that the chewing process plays an integral role in the release of digestive enzymes as well as breaking down food into particles of an ideal size to be further digested in the gut.
11. Augment Your Supply of Digestive Enzymes
While our bodies do naturally produce digestive enzymes, research suggests that it's common for individuals to produce decreased quantities. Levels of hydrochloric acid, specifically, seem prone to dropping with age.
If you do wish to try digestive enzyme supplements, you should choose a broad-based multi-enzyme formula. There may be some additional benefits from choosing one that contains betaine HCI; however, some find that formulation gives them heartburn.
12. Liberalize Healthy Fats
As you're likely aware, omega-3 fatty acids have impressive anti-inflammatory capacities. This enhances gut health as well as overall health. Good sources of omega-3s include many types of fish and seeds as well as the burgeoning superfood algae.
Short-chain fatty acids and medium-chain fatty acids from whole food sources also help to fight inflammation. Fats found in olives, avocados, and coconuts, as well as some nuts and seeds, have proved to be powerful allies.
13. Check Your Vitamin D and Iron Levels
Deficiencies in either of these key nutrients can adversely impact gut health.
Low levels of vitamin D impair immune function and have been associated with an increased prevalence of irritable bowel disease.
Low levels of iron are also linked to impaired gut function. The underlying cause of an iron deficiency may by gut malabsorption, excessive consumption of mineral-binding foods like grains and legumes, or a failure to meet the requirements for dietary iron intake.
14. Add Supplements as Needed
The most effective way to address poor gut health is to ascertain the underlying cause and address it.
In some cases, however, it can be helpful to integrate natural compounds either as you navigate that process or in order to counterbalance electrical or structural digestive issues.
Some supplements to consider include: St. John’s Wort, melatonin, curcumin (turmeric), Iberis amara, chamomile, arrowroot, peppermint, Boswellia carterii, artichoke leaf, clove, zinc, quercetin, gamma oryzanol, licorice root, CoQ10, phosphatidylcholine, aloe vera, and psyllium. The specifics of your situation will inform which of these, if any, is the best fit for you.
15. Prioritize Glutamine Intake
Glutamine, a nonessential amino acid, is a unique nutrient that (as touched on previously) provides fuel for metabolism, regulates cell proliferation, and repairs and maintains gut barrier function.
Your gut needs glutamine in order to transport nutrients into the blood and restock cells. Not only is glutamine a crucial source of energy for intestinal cells, but it also has the ability to reverse inappropriate gut permeability. When enough glutamine is available, in conjunction with a host of growth factors and regulatory peptides that play protective and healing roles, the gastrointestinal mucosal integrity is quickly restored. Glutamine may even help alleviate allergic responses to various food compounds.
Glutamine is the most abundant amino acid in blood and, while the body can synthesize it, it is a conditionally essential amino acid. Glutamine becomes essential when, during catabolic stress or exposure to pathogens, the rate at which it is used to fuel and rebuild the mucosa is greater than the rate at which the body can produce new glutamine.
If you're experiencing chronic symptoms of poor gut health, you can likely benefit from an increased intake of glutamine.
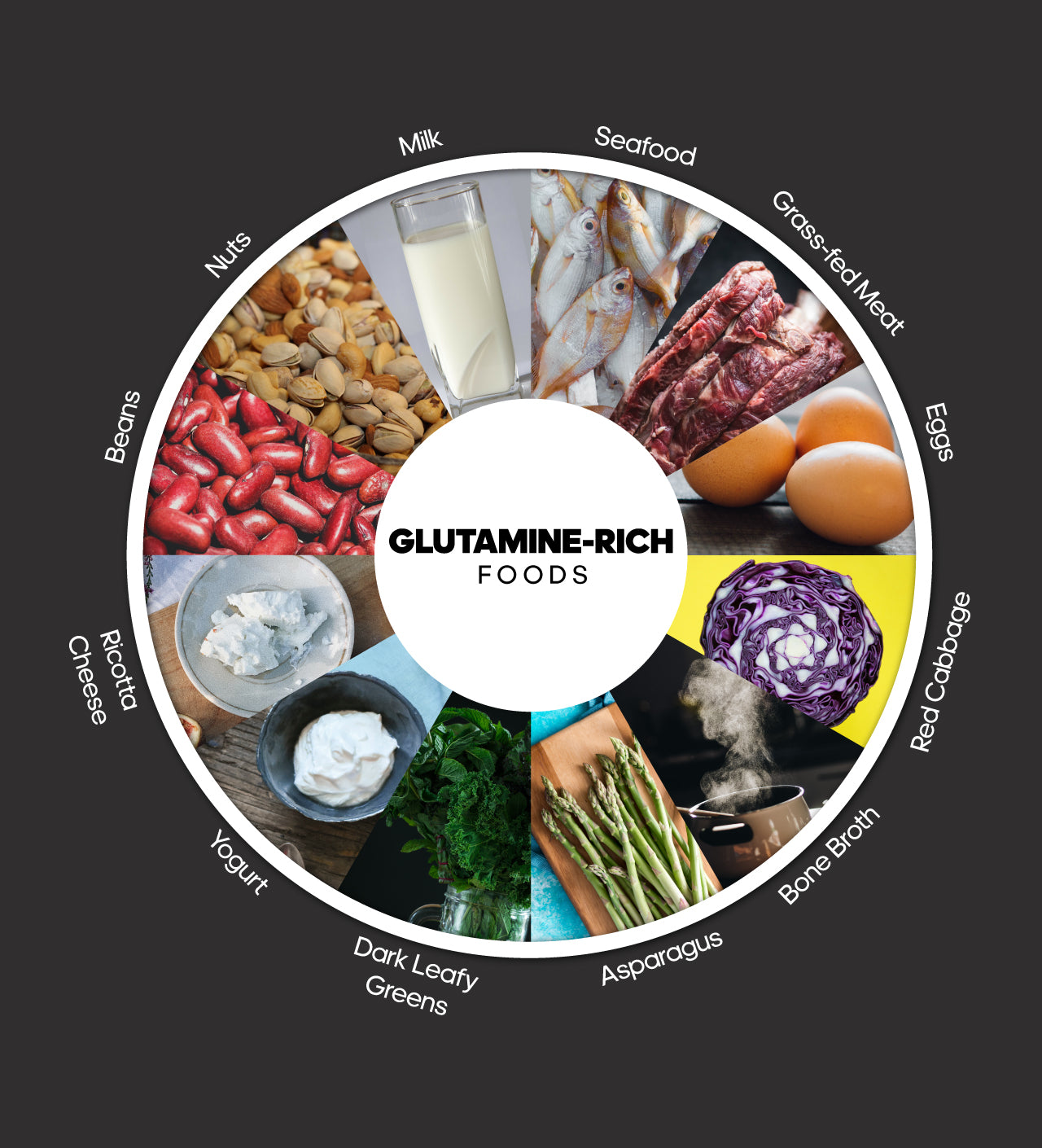
No one nutrient can cure all digestive woes, but adding glutamine-rich foods to your diet is a great first step toward better gut health.

Up to 25% off Amino
Shop NowTAGS: diet plans food
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















