Everything You Need to Know About Scoliosis
 By: by Amino Science
By: by Amino Science

Even the most normal spine has some degree of curvature, but the spinal cords of individuals with scoliosis curve far too much. Scoliosis can affect people of all ages, from babies to adults, but it most often appears in late childhood just prior to the onset of puberty.
In most cases, scoliosis in children and adolescents does not require treatment, as the exaggerated spinal curve corrects itself during their continued growth process. Depending on the degree of curvature of the spine as well as the age at the time of diagnosis, doctors may recommend a combination of bracing and physical therapy exercises.
To treat severe scoliosis, surgery may be required. Scoliosis surgery can come with complications including chronic pain, decreased respiratory capacity, and limitations to physical movement, so it's only used when the benefits outweigh the risks.
In this article, we’ll take a closer look at this condition and share everything you need to know about scoliosis, from risk factors to symptoms of scoliosis to the best ways to treat each type of scoliosis.
What Is Scoliosis?
Scoliosis (pronounced sko-lee-o-sis) occurs when the spine has a sideways curvature. In order to be classified as scoliosis, the curvature of the spine must be greater than 10 degrees on an x-ray, resulting in a S or C shape. It can affect any section of the spine but is most often seen in the lower back and directly behind the chest. The bones in a scoliotic spine may also have rotated slightly, which can make a person's waist or shoulders look uneven.
Scoliosis can develop at any point from infancy to adulthood. It is most frequently seen in children who have yet to reach puberty, around 10 to 12 years old. Scoliosis sometimes coincides with a growth spurt and appears more often in girls than in boys. Treatment is not always necessary for mild cases, and most people are able to participate in all kinds of physical activities without complications and live fulfilling, unrestricted lives.
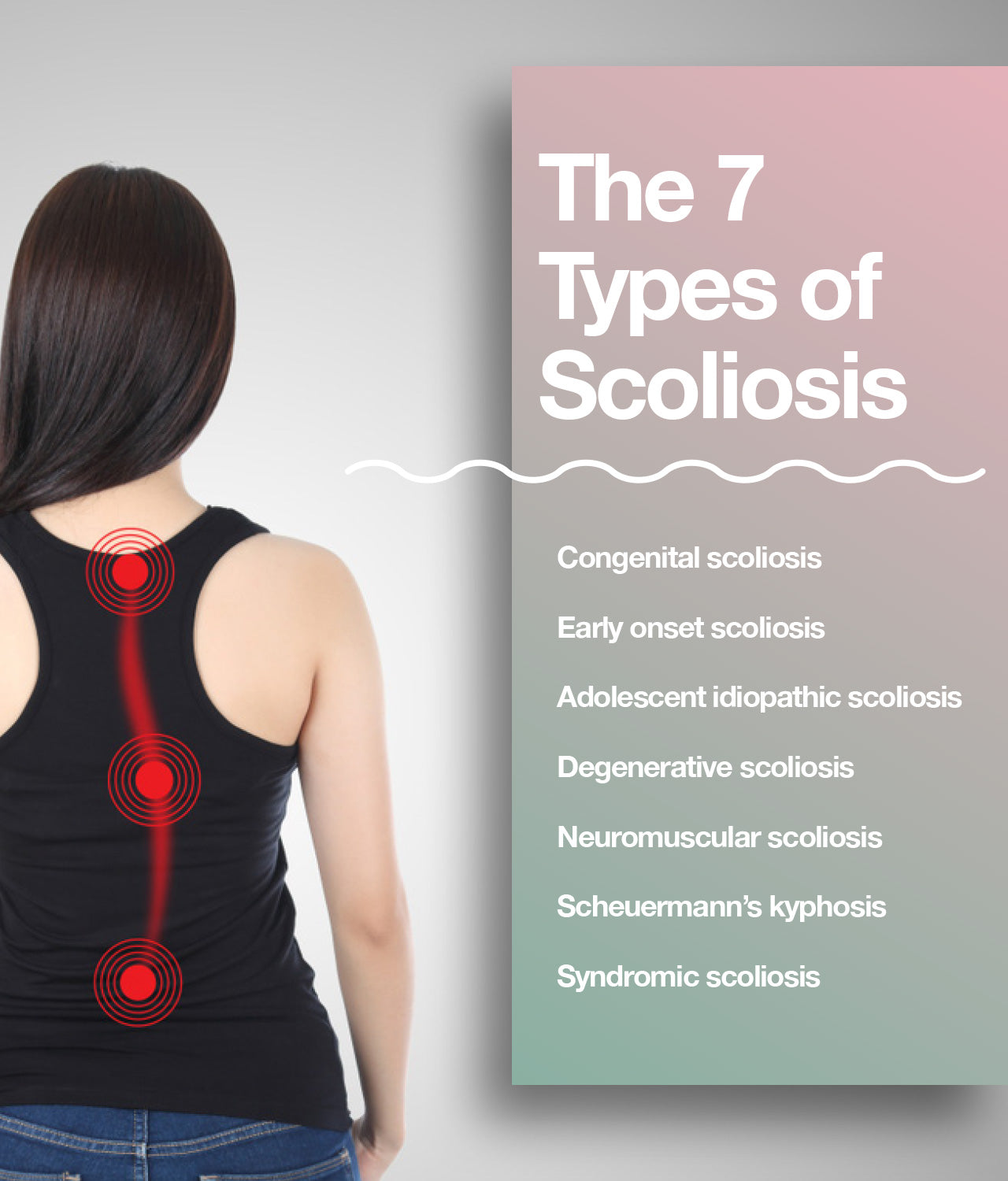
The 7 Types of Scoliosis
By far the most common type of scoliosis is what's called idiopathic scoliosis, which means, essentially, "of no known cause." According to the Scoliosis Research Society, more than 80% of all cases of scoliosis fall into this category.
That said, experts have identified seven types of scoliosis:
- Congenital scoliosis: Occurs when the spine forms abnormally during fetal development. This type of scoliosis is present from birth.
- Early onset scoliosis: When a spinal curve appears at any time from birth until 10 years of age, or prior to the onset of puberty, that's classified as early onset scoliosis. This type of scoliosis is often idiopathic.
- Adolescent idiopathic scoliosis: Similar to early onset scoliosis, but differentiated by the fact that it presents during or after puberty. The spine curves sideways and twists, which can pull the ribcage out of alignment. This type also tends to be idiopathic.
- Degenerative scoliosis: Seen in adults when the spine and bones have worn down or been damaged. This degeneration creates pressure that can cause the spine to curve. Degenerative scoliosis can affect individuals with or without a history of scoliosis.
- Neuromuscular scoliosis: Neurological or muscular conditions including Duchenne muscular dystrophy and cerebral palsy can impact the muscles surrounding the spine and cause it to gradually collapse. Frequently, the spinal curves created by this type of scoliosis are progressive, meaning they become more severe over time.
- Scheuermann’s kyphosis: A rare type of scoliosis that usually presents between age 10 and age 15 and causes abnormal growth of certain areas of the spine where vertebrae wedge forward during development. The exact number of individuals affected by Scheurmann's kyphosis is not known because it can easily be mistaken for poor posture.
- Syndromic scoliosis: Refers to spinal abnormalities caused by genetic conditions or pre-existing disorders. This type of scoliosis is most likely to co-occur with connective tissue disorders such as Marfan's and Ehlers-Danlos syndrome as well as trisomy21, Prader-Willi syndrome, Rett syndrome, and Beals syndrome.
The Truth About the Causes of Scoliosis
What causes scoliosis is not always easy to pinpoint. As touched on in the preceding section, statistics show that the cause of scoliosis cannot be identified in 8 out of 10 cases. While some instances may be linked to an undiagnosed underlying condition, meaning they would be properly categorized as syndromic scoliosis, many of them are simply the result of genetics.
Around 3 in 10 young adults with idiopathic scoliosis have a family history of the condition, according to the American Academy of Orthopedic Surgeons. This can cause scoliosis to develop during gestation or much later in life when wear and tear weakens a spine predisposed to twist and curve. A multitude of other causes can play into the development of scoliosis, including infections or fractures involving the spine.
Perhaps because it can be so frustrating trying to identify the cause of scoliosis, many misconceptions and false assumptions have cropped up about possible causes. Despite what some misleading sources claim, none of the following factors contribute to the development of scoliosis:
- Carrying a heavy bag
- Athletic endeavors
- Poor posture
- Calcium deficiency
- Minor leg length differences
Identifying Symptoms of Scoliosis
Signs of scoliosis are not always obvious at first and may gradually appear over time. Especially in young individuals, the condition is often missed until a growth spurt. In adults, many back issues may be blamed on other conditions like arthritis and an accurate diagnosis may be delayed. Identifying scoliosis early can be crucial when it comes to remedying the problem before it worsens and results in more serious issues.
Typically the mild curves that present during the early stages of scoliosis do not cause pain, but individuals may experience discomfort if they overcompensate for the parts of the skeleton that are off balance by standing or walking awkwardly. Back pain can become more persistent if the spine continues to curve and the condition worsens.
The precise symptoms of scoliosis vary depending on the age at which the condition presents. When scoliosis presents in late childhood, adolescence, or adulthood, some indicators to look for include:
- Protruding hip on one side
- Head not centered, leans to the side
- Ribs not even and may be at different heights
- One shoulder, or shoulder blade, higher than the other
- Clothes hang asymmetrically
- One leg longer than the other
- Overall tilt to one side while standing
When scoliosis appears in infancy, however, key symptoms to look for include:
- Bulge on one side of the chest
- Consistent curving to one side while lying down
- Shortness of breath
- Chest pain
- Issues with heart and lungs
How to Treat Scoliosis
To develop a treatment plan for scoliosis, a doctor will conduct a physical examination of the spine, shoulders, head, ribs, and hips. An instrument called a scoliometer, or inclinometer, can measure the asymmetry of the spine in degrees. While you are bending forward, the doctor will place the scoliometer over the spine and take the measurement.
Imaging scans such as x-rays, CT scans, and MRIs may also be used to assess the shape, direction, location, and angle of the curve.
The earlier scoliosis is treated the better, but the exact plan of action depends on how old you are, the current condition of the spine, and whether a doctor believes the curve could worsen as time goes on.
There are two types of spinal curves: structural curves and nonstructural curves. Structural curves are permanent while nonstructural curves are temporary and will most likely resolve with time.
Often, children with scoliosis have mild, nonstructural curves that do not require treatment. In these cases, a doctor will often recommend following up every 4 to 6 months to monitor the curve of the spine in clinic and periodically with x-rays.
When deciding on treatment options, a doctor takes into consideration the following factors:
- Age: Once a person's bones have stopped growing, it becomes less likely that his or her spinal curve will become more severe. However, treatments like braces work more effectively while the bones are still maturing.
- Sex: Females have a higher risk than males of having their spinal curves become progressively more severe.
- Severity of the curve: The greater the spinal curvature to begin with, the more likely it will worsen over time.
- Shape of the curve: Curves that take the shape of the letter S, sometimes called double curves, have a higher probability of becoming more severe over time than curves shaped like the letter C.
- Position of curve: Curves in the lower and upper sections of the back tend to be more stable while those in the center of the spine tend to worsen.
Mild scoliosis can often be treated with exercises, such as yoga and targeted stretching, that strengthen the spine and surrounding muscles. This treatment approach should be guided by a doctor who will monitor progress closely to look for changes and to see if these self-care practices improve the condition.
The specific exercises used to treat scoliosis vary depending on which school of thought the practitioner in question follows. That said, the goals of all the exercises remains consistent: to realign the spine, rib cage, shoulders, and pelvis so that a correct, upright posture can be achieved.
If a doctor determines that a more aggressive treatment is needed, there are three basics approaches to consider.

1. Back Brace
For cases of scoliosis that require more serious medical intervention than at-home exercises, a doctor may suggest a back brace to stop, or slow, the worsening of the spinal curvature.
This method is most helpful in younger patients whose skeleton is still developing. It does not change the shape of the spine, but instead prevents further changes while the person continues to grow. It's typical for these types of braces to need to be worn consistently throughout the day and night in order reap the biggest benefits. Doctors usually recommend that they only be removed for bathing. The more hours a day a patient wears the brace, the better the results will be.
The braces available today do not overly restrict movement, but may need to be taken off to allow for participating in sports and other types of physical activity. One study found that when bracing is used on young adults with idiopathic scoliosis, it helped minimize the chances of the condition worsening or requiring surgical treatment.
There are two basic types of braces:
- Thoracolumbosacral orthosis (TLSO): Made from plastic and designed to fit neatly around the body, this type of brace is typically not visible under clothing.
- Milwaukee brace: A full-torso brace including a neck ring with supports for the chin and back of the head. This type of brace is only used when the TLSO is not an option or has not been effective.
Once the bones have fully matured, the use of braces can be discontinued.
2. Casting
This can be a very helpful treatment approach in infants and young children as, unlike bracing, it can actually correct spinal curvature, especially when done at a very early age and in those with smaller curvatures. The age cap can go up to 10 years, but most practitioners are reluctant to cast after age 6. Doctors mold plaster casts around the outside of the body. The casts must be regularly updated—on average, every 2 to 3 months—to allow for the child's growth.
The benefit of casting is that it helps the spine grow straighter and ensures the lungs and chest have space to develop correctly. It can slow or eliminate the need for surgery.
3. Surgery
Surgery is the last recourse, to be used when all other measures have been exhausted. However, when the curvature has become too great or symptoms too disruptive, spinal surgery becomes the best option.
The specific surgical treatment is determined based upon the shape of the spine, height, and whether or not other areas of the body are negatively affected by the spine’s shape and curve.
Spinal surgery may involve:
- Spinal fusion: Using new bone grafts, two or more of your vertebrae are fused together. Parts of your spine can also be held together by wires, screws, metal rods, or hooks to allow the bones to heal properly.
- Intensive care: A spinal surgery can take between 4 and 8 hours, meaning intensive post-operative care will be required. This will involve monitoring in the ICU for 24 hours, providing medication to help relieve pain, and IV fluid to maintain hydration and encourage healing. For more serious conditions or complicated surgeries, a longer hospital stay may be necessary.
- Recovery: Recovery time varies, but in most cases, it's possible to return to normal activities within a month. Sports and other contact activities are typically postponed for at least a year to ensure the spine is able to heal properly. Doctors may recommend a supportive back brace during the first few months following surgery. Heal is a surgical recovery supplement proven to improve physical strength and function as measured at 6 weeks post surgery. Click here to learn more.
In childhood cases, the rods will need to be extended every 6 months to account for growth. This does not require being admitted into the hospital and can be done during a daytime office visit. Once the spine has fully developed, the rods are removed via surgery.
The best approach to scoliosis is a proactive one that involves practicing regular exercises and working with a doctor to take preventative measures. It is possible to slow spine curvature and minimize any associated symptoms. Activities like yoga and pilates can greatly improve flexibility, strengthen muscles that support the spine, and enhance overall health and wellness.


Up to 25% off Amino
Shop NowTAGS: conditions
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















