5 Factors That Raise Your Risk for Liver Disease
 By: by Amino Science
By: by Amino Science

The most regenerative of all the organs, the liver can sometimes be taken for granted. We flood it with alcohol, medications, hidden toxins in our environment, and expect it to work tirelessly filtering our blood, warding off infections, and producing bile for digestion. But the liver isn’t indestructible. Treat it with care by staying vigilant of these 5 factors that raise your risk of liver disease.
A Brief Introduction to Liver Disease
Before we explore the reasons why you may be at risk for liver disease, let’s set the stage with some liver basics.
This football-sized organ sits just under the rib cage at the right side of your abdomen and is responsible for removing toxins from the blood, breaking down alcohol, fats, and medications, producing infection-fighting hormones, enzymes, and proteins, converting nutrients from the food we eat into usable substances for the body, storing glycogen for energy, and generating bile for digestion.
The liver has many potential enemies thwarting its well-being and causing damage that can progress to scarring (cirrhosis of the liver), eventual liver failure and, if a liver transplant is not found, possible death.
Leading Causes of Liver Disease
- Heredity: Along with a family history of liver disease, an abnormal gene passed along from one or both parents can lead to the accumulation of harmful substances in the liver. Inherited disorders include Wilson’s disease, hemochromatosis, and alpha-1 antitrypsin deficiency.
- Parasites and viruses: Viral infections such as hepatitis A, hepatitis B, and hepatitis C, spread through blood, bodily fluid, contaminated food or water, or close person-to-person contact, and can stoke inflammation that brings on liver damage.
- Autoimmune conditions: These disorders can cause the immune system to act uncharacteristically and attack healthy organs that affect liver function. Autoimmune conditions implicated in liver damage include autoimmune hepatitis, primary biliary cirrhosis, and primary sclerosing cholangitis.
- Cancer: All roads lead to the liver, leaving it susceptible to cancer cells traveling through the bloodstream. Primary liver cancer from hepatitis viruses account for just 2% of cancers in America, while most liver cancers arise from cancer in other parts of the body.
- Chronic alcohol abuse: Up to 20% of heavy drinkers will develop fatty liver disease. That’s because excessive alcohol use destroys liver cells, causes scarring and inflammation of liver tissue (called alcoholic hepatitis), as well as cellular mutation that can lead to liver cancer.
- Fat buildup in the liver: Alcohol isn’t the only substance that can cause fat to accumulate in the liver. Non-alcoholic fatty liver disease (NAFLD) is associated with type 2 diabetes and obesity. If not detected and treated early, NAFLD can progress to end-stage liver disease.
- Over-the-counter and prescription medications: These medications are processed in the liver, and continued use can tax an overworked liver. Herbal supplements can also overburden the liver. Read on for our list of liver-compromising medications and supplements below!
Symptoms of Liver Disease
Liver disease can be managed and sometimes reversed if caught early. Stay watchful for the following signs of liver damage:
- Yellowing of the skin and eyes (a condition called jaundice)
- Swelling in the abdomen, legs, and ankles
- Dark urine
- Pale, tar-colored stool
- Itchy skin
- Exhaustion or chronic fatigue
- Nausea and vomiting
- Bruising
- Weakness
- Disorientation
Liver disease can, however, be present without any noticeable symptoms. For this reason it’s important to get regular blood tests, as elevated liver enzymes can indicate liver trouble. If you suspect liver problems, a visit to a liver specialist may be in order. New technology allows your health care provider to observe the concentration of fat in your liver and check for stiffness, which is a sign of scarring.
5 Ways to Increase Your Risk for Liver Disease
1. Chronic Alcohol Abuse
Let’s start with the most well-known risk factor for chronic liver disease: excessive alcohol consumption.
The liver is responsible for processing 90% of the alcohol we consume. One drink takes about an hour of work. However, when we add to that burden with two, three, or more drinks, the liver takes longer to filter the alcohol and can’t always keep up. Unprocessed alcohol builds up in the bloodstream and makes its way to the heart and brain; hence, the intoxicating side effects. When experienced over and over again, liver cells eventually give out and alcoholic hepatitis emerges, along with eventual liver degeneration.
All of this is avoidable by following moderate drinking guidelines:
- No more than 1 drink a day for women
- No more than 2 drinks a day for men
When you go over 8 drinks a week for women and 15 drinks for men, you’ve entered high risk territory. Find out exactly what happens when your liver is exposed to alcohol here.
2. Exposure to Toxins
Chemicals enter our bloodstreams and are eventually broken down by the liver, but the process introduces byproducts that, with constant exposure, can wear down the liver’s regenerative capacity. Industrial chemicals including dry cleaning solvent, tetrachloride, vinyl chloride that is used to make plastics, polychlorinated biphenyls, and the herbicide Paraquat, to name a few, put painters, chemists, dry cleaners, farm workers, printers, and health care workers at risk.
Along with alcohol and the use of certain medications and supplements (see below), exposure to these toxins can cause toxic hepatitis, a form of liver inflammation that can develop in a few hours or after several months of exposure.
Stay safe by wearing protective coverings, gloves, long sleeves, and face masks when spraying insecticides and fungicides, or painting, and make sure your environment is well ventilated.
3. Medications and Supplements
Frequent intake of certain medications and supplements have similar effects on the liver as alcohol intake and exposure to toxins do. In fact, OTCs, prescription medications, and dietary supplements are implicated as the most common cause of acute liver failure, which is the rapid deterioration of liver function.
When taken too much or with alcohol, over-the-counter pain relievers to be wary of include:
- Acetaminophen (Tylenol)
- Nonsteroidal anti-inflammatories
- Ibuprofen (Advil, Motrin)
- Naproxen (Aleve)
- Salicylate (Aspirin)
As for prescription medications, statins used to treat high cholesterol have come under fire, as have:
- Antibiotics (amoxicillin-clavulanate, erythromycin)
- Arthritis drugs (methotrexate, azathioprine)
- Antifungal drugs
- Niacin
- Steroids
- Allopurinol for gout
- Antiviral drugs for HIV infection
And supplements, a highly unregulated industry, must also be taken with caution, as certain herbs can adversely affect the liver when consumed too frequently or in too high a dose. Exercise caution when using:
- Black cohosh
- Kava
- Aloe vera
- Ephedra
- Cascara
- Chaparral
- Comfrey
For a more complete list of OTCs, prescription medications, and herbal supplements that have been linked to liver toxicity, refer to the LiverTox database.
4. Type 2 Diabetes and Obesity
Obesity and type 2 diabetes more often than not go hand in hand. Obesity raises your risk of developing type 2 diabetes by as much as 85%, and both conditions impact your liver via the same mechanism—a reduced sensitivity to insulin.
One of the liver’s most important jobs is to keep blood sugar levels balanced. When too much fat accumulates in the liver, it cannot monitor insulin as effectively, and glucose builds up in the blood, paving the way for type 2 diabetes. Research shows that 75% of individuals with prediabetes or type 2 diabetes have a buildup of liver fat, and nearly half of those have scar tissue.
Once diabetes takes hold, your odds of developing a more aggressive form of NAFLD called nonalcoholic steatohepatitis (NASH) increase. Inflammation and fat have built up to such a degree that scarring has occurred, and, if not treated, will advance to liver cirrhosis and end-stage liver disease.
There is a way to reverse that damage if caught and checked early enough! Losing as little as 10% of your body weight can stop NAFLD and NASH from progressing.
5. Unprotected Sex and Unsterile Needles
There are 5 types of hepatitis viruses, but in the United States hepatitis A, hepatitis B, and hepatitis C infections are the most common, and they can all be transmitted through unprotected sex and lead to chronic hepatitis, causing liver inflammation and ushering in irreparable damage.
Condoms can protect against 99% of sexually transmitted diseases (STDs), including hepatitis viruses.
Illicit use of intravenous drugs also puts you at increased risk for the hep C virus and hep B virus, and more rarely the hep A virus. Getting tattoos or body piercings from unlicensed and unprofessional tattoo parlors can also leave you vulnerable to viral hepatitis.
Seek help if you are participating in illicit drug use and sharing needles with others, and be sure to get tattoos and piercings from reputable businesses that take the necessary precautions to ensure their equipment is sterile and their practices sanitary.
COVID-19 and the Liver
According to the Centers for Disease Control and Prevention (CDC) some coronavirus patients have elevated liver enzyme concentrations, which signal a certain degree of liver damage. And patients with more severe reactions to the virus also exhibit liver damage, although the exact cause is still under investigation.
The CDC also states that it is unknown whether people with the hepatitis C virus or hepatitis B virus, cirrhosis, fatty liver, liver cancer (hepatocellular carcinoma), or other liver conditions have a higher risk of COVID-related liver damage.
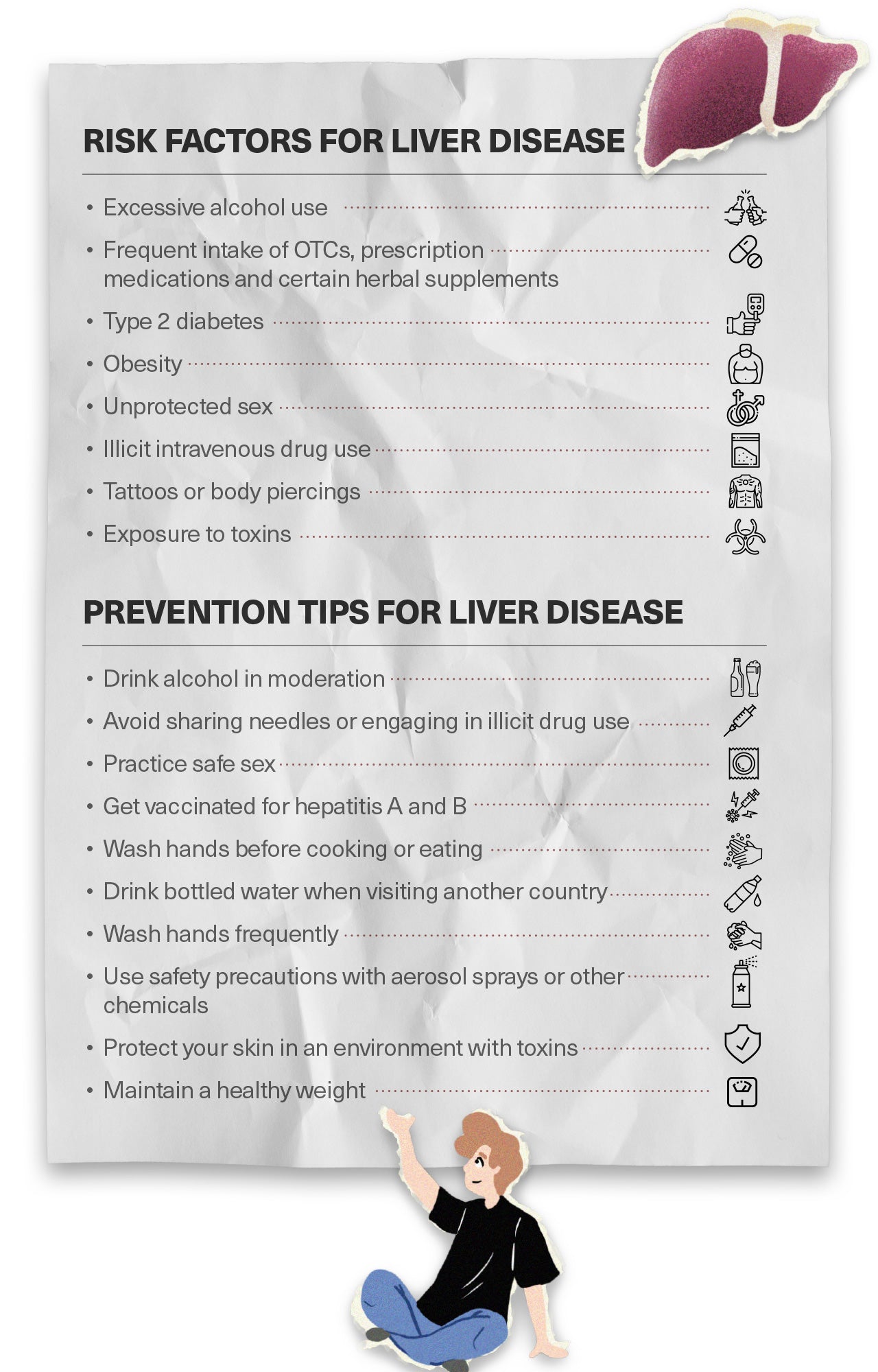
Liver Disease Prevention Tips
You’ve probably picked up a few ways to reduce your risk for liver disease already. Here’s a recap:
- Drink alcohol in moderation
- Avoid sharing needles or engaging in illicit drug use
- Practice safe sex
- Get vaccinated for hepatitis A and B
- Wash hands before cooking or eating
- Drink bottled water when visiting another country
- Wash hands frequently
- Use safety precautions with aerosol sprays or other chemicals
- Protect your skin in an environment with toxins
- Commit to a weight-loss program
- Maintain a healthy weight
There is one prevention and treatment tip we haven’t yet covered—supplementing with essential amino acids.
How can the building blocks of protein help protect and heal the liver?
Taking just 13 grams of essential amino acids twice a day for a month has been shown to lower liver fat levels in people with mild to moderate alcohol use disorder (1).
Taking essential amino acids orally has also been shown to protect against the accumulation of liver fat in people who eat a high sugar diet, as well as those with high cholesterol (2).
An essential amino acid supplement helps protect against all manner of disease, including heart disease and sarcopenia, as well as speed recovery from illness, injury, or surgery.
To learn more about how amino acids and other natural strategies can help protect against and reverse liver disease, keep reading here! And to start supplementing with a targeted liver health formula, click here.

Up to 25% off Amino
Shop NowTAGS: liver
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620



















