The Truth Behind the Apple Cider Vinegar Fatty Liver Detox, Plus Science-Based Advice on Improving Liver Health
 By: by Amino Science
By: by Amino Science

Given that pharmaceutical companies have yet to devise a drug to treat fatty liver disease, it's hardly surprising how much interest there is in natural remedies for this condition. One popular example of this type of home remedy is the apple cider vinegar fatty liver detox. Advocates claim that conducting a cleanse with apple cider vinegar helps to flush toxins from the body, regulate blood sugar levels, and encourage healthy weight loss, all of which can improve liver health. However, there's little scientific support for these claims.
Read on for clear, evidence-based information about fatty liver disease, why some people believe apple cider vinegar can effectively treat this condition, and what steps to take to protect and improve your liver health.
What Is Fatty Liver Disease?
Before describing fatty liver disease, let's establish what normal, healthy liver function looks like. The liver, the largest of the internal organs, carries out a host of absolutely vital functions, such as:
- Cleansing toxins from the bloodstream
- Metabolizing nutrients
- Processing lipids and amino acids
When you consume foods that contain protein, your liver uses enzymes (specifically, deaminases and transaminases) to convert the amino acids your body absorbs from the protein into the most bioavailable, utilizable forms. The liver also converts excess carbohydrates into fatty acids and other substances that the body can use as energy sources or store as fat to be used at a later date. A small percentage of those fat molecules get stored in the liver itself.
Factors such as chronic alcohol abuse, long-term drug use, nutritional deficiencies, and metabolic disorders can all interfere with your liver's ability to fulfill its many essential functions. One of the ways this manifests is that the liver begins to increase the amount of fat stored in its cells. At the moment the amount of fat stored in the liver reaches the threshold of 5% to 10% of total liver volume, an official diagnosis of fatty liver disease (or hepatic steatosis) can be made.
The Two Main Types of Fatty Liver Disease
Though the physical effects of fatty liver disease remain consistent across types, it's valuable to have an understanding of the different pathophysiologies, as that influences how the body responds to treatment.
There are two primary types of fatty liver disease: alcoholic fatty liver disease and nonalcoholic fatty liver disease.
Alcoholic Fatty Liver Disease
As the name indicates, alcoholic fatty liver disease arises due to long-term alcohol abuse. Scientists have known for centuries that over-consumption of alcohol leads to liver disease. The majority of the metabolization of alcohol transpires in the liver, making it quite susceptible to alcohol-related injury.
In the first stage of alcoholic liver disease (also called alcoholic steatohepatitis), the liver begins to struggle to break down fatty acids. This can result in high serum triglyceride levels, inflammation of the liver (alcoholic hepatitis), and the development of scars in the liver tissue (cirrhosis).
Early intervention can, in some cases, allow the liver to cleanse itself, thereby naturally reversing the buildup of fat. Subsequently, it can function normally once more. Refraining from the consumption of all types of alcohol for a 2-week period can be sufficient, if this step is taken shortly after liver dysfunction sets in.
The longer the accumulation of fat in the liver goes on, the more extensive the related damage, and the greater the likelihood of long-term impairment of liver function, permanent scarring, and liver failure.
Nonalcoholic Fatty Liver Disease
Alcohol consumption is not the only risk factor for the development of liver disease. Other health considerations can also cause fat to build up in the liver, such as:
- Family history of type 2 diabetes
- Aging
- Increased body weight, particularly the development of deposits of belly fat
These can also interfere with the body's insulin sensitivity, and when the body does not properly register the presence of insulin, it responds to the perceived deficit by accelerating its innate insulin production process. This results in elevated insulin levels, which can set off a cascade of ill-effects, including high blood pressure, elevated serum triglyceride levels, and—you guessed it—the accumulation of fat in the liver.
Nonalcholic fatty liver disease (NAFLD) can be limited to the presence of excess fat in the liver, with very little inflammation and liver damage apart from that, or it can progress to non-alcoholic steatohepatitis (NASH), which involves both liver inflammation and damage. As is the case for liver disease stemming from alcohol abuse, NAFLD and NASH can progress to cirrhosis and liver failure. Experts estimate that between 80 and 100 million Americans have NAFLD, though many of them are not aware of that due to the fact that it's largely asymptomatic.

Diagnosing Fatty Liver Disease
Because the early stages of fatty liver disease are often unaccompanied by clear physical indicators, many people do not realize they have the condition until it's progressed to a more advanced stage or until unrelated medical tests reveal liver dysfunction.
The challenge of detecting fatty liver disease is increased by the fact that blood tests, one of the most common methods of screening for chronic diseases, do not always accurately reflect the health of the liver. Fatty liver disease can cause liver enzyme levels to become elevated, but it's also entirely possible for individuals with liver disease to have entirely normal enzyme levels, even when the disease progresses to the point of cirrhosis.
Ultrasound may be a more reliable way to diagnose fatty liver, according to a 2018 hospital-based, cross-sectional study published in the Journal of International Medical Research. The authors state that ultrasound's "sensitivity and specificity in detecting moderate to severe fatty liver are comparable to those of histology
Signs and Symptoms of Fatty Liver Disease
As fatty liver disease advances and liver function becomes increasingly poor, signs and symptoms do begin to appear. One clear indication of liver disease is altered amino acid metabolism—because of this, supplementing with amino acids (particularly, branched-chain amino acids) can significantly enhance liver health. We'll share more on that later in the section on proven treatments for fatty liver disease, but first, let's go over other indicators of liver disease.
Clinical evidence indicates that the following symptoms may point to the presence of liver disease.
- Pain and tenderness in the upper-right abdomen, due to liver enlargement
- Loss of appetite
- Weight loss
- Weakness
- Fatigue
- Jaundice (yellowing of the skin and eyes)
- Weakness
- Itchiness
- Nosebleeds
- Spider veins (clusters of blood vessels that resemble spider webs)
- Confusion and difficulty focusing
- Ascites (abdominal pain and swelling)
- Edema (swelling of the legs)
- Gynecomastia
What Is the Apple Cider Vinegar Fatty Liver Detox?
If you're serious about improving the health of your liver, you have likely looked into various liver cleanses. There's little data to support the supposed beneficial effects associated with several players in this realm, including lemon juice, green tea, olive oil, and apple cider vinegar (ACV).
Made from apples that have been mashed, distilled, and fermented, apple cider vinegar has been rumored to have detoxifying properties for centuries. As scientists have analyzed apple cider vinegar's efficacy as a treatment for a wide range of conditions, they've concluded that the high levels of acetic acid and other compounds it contains may indeed influence human health, though exactly how they do so remains somewhat obscure.
Advocates of the detoxifying properties of apple cider vinegar claim that it can:
- Flush toxins from the body
- Facilitate weight loss
- Bring the body's pH into balance
- Even out blood sugar levels
- Drop high cholesterol into the healthy range
Given that, it's understandable why those same advocates would believe you can use apple cider vinegar to treat fatty liver disease.
Scientific Studies on Apple Cider Vinegar and Liver Health
Researchers have confirmed that the substances we eat and drink can both improve and undermine the body's natural detoxification processes. What's less clear, however, is whether apple cider vinegar specifically has a beneficial impact on liver health.
Some research has been conducted on proposed ACV benefits relevant to liver health, but the results are far from conclusive.
Weight Loss
This is perhaps the most hyped benefit of apple cider vinegar. Much of the excitement surrounding ACV's weight-loss benefits can be traced back to a 2009 study done by a Japanese research team. The researchers found that daily consumption of vinegar resulted in modest reductions to:
- Body weight
- Visceral and subcutaneous fat mass
- Serum triglyceride levels
However, the study did not look at the use of ACV in particular (though the researchers did cite ascetic acid and previous animal studies on its benefits).
A very small study from 2007 looked at the effect of apple cider vinegar on gastric emptying rate (GER) for 10 individuals with type 1 diabetes. They found that participants who paired a cup of water with 2 tablespoons of ACV mixed in with their serving of pudding had slower rates of gastric emptying than those who simply drank a cup of water. Slower gastric empyting can correlate with increased fullness, which can in turn led to weight loss. However, as the study authors themselves noted in their conclusion: "Clearly, a larger, randomized trial involving a greater number of patients would be needed to validate the findings of this pilot study."
All in all, the enthusiasm about apple cider vinegar's ability to encourage weight loss has yet to be corroborated by hard facts.
Cholesterol Levels
As we touched on in the previous section, the 2009 study did find some improvements to cholesterol levels, specifically, to serum triglyceride levels. However, that was not the primary focus of the study.
A small Iranian study that enrolled 19 participants with hyperlipidemia (high cholesterol levels) found that 8 weeks of apple cider vinegar consumption "significantly reduced harmful lipids, i.e., total cholesterol, LDL, and triglyceride, in blood samples of hyperlipidemic individuals who had never used any lipid-lowering drugs."
While those are certainly promising results, further studies with larger and more diverse enrollment need to be conducted before arriving at firm conclusions about ACV's impact on cholesterol levels.
Blood Sugar Regulation
There's some evidence to suggest that drinking apple cider vinegar can prevent blood sugar spikes associated with carbohydrate consumption. Controlling blood sugar levels is of paramount importance for individuals with diabetes, who also face a higher risk of developing nonalcoholic fatty liver disease.
A small study that enrolled four men and seven women with type 2 diabetes (all of whom were not taking insulin to control their condition) found that ingesting apple cider vinegar before bedtime had a favorable effect on waking glucose levels. However, as is true of the studies on the benefits of ACV cited in the earlier sections, the findings are limited by the study's small sample size.
Negative Side Effects Associated with the Apple Cider Vinegar Fatty Liver Detox
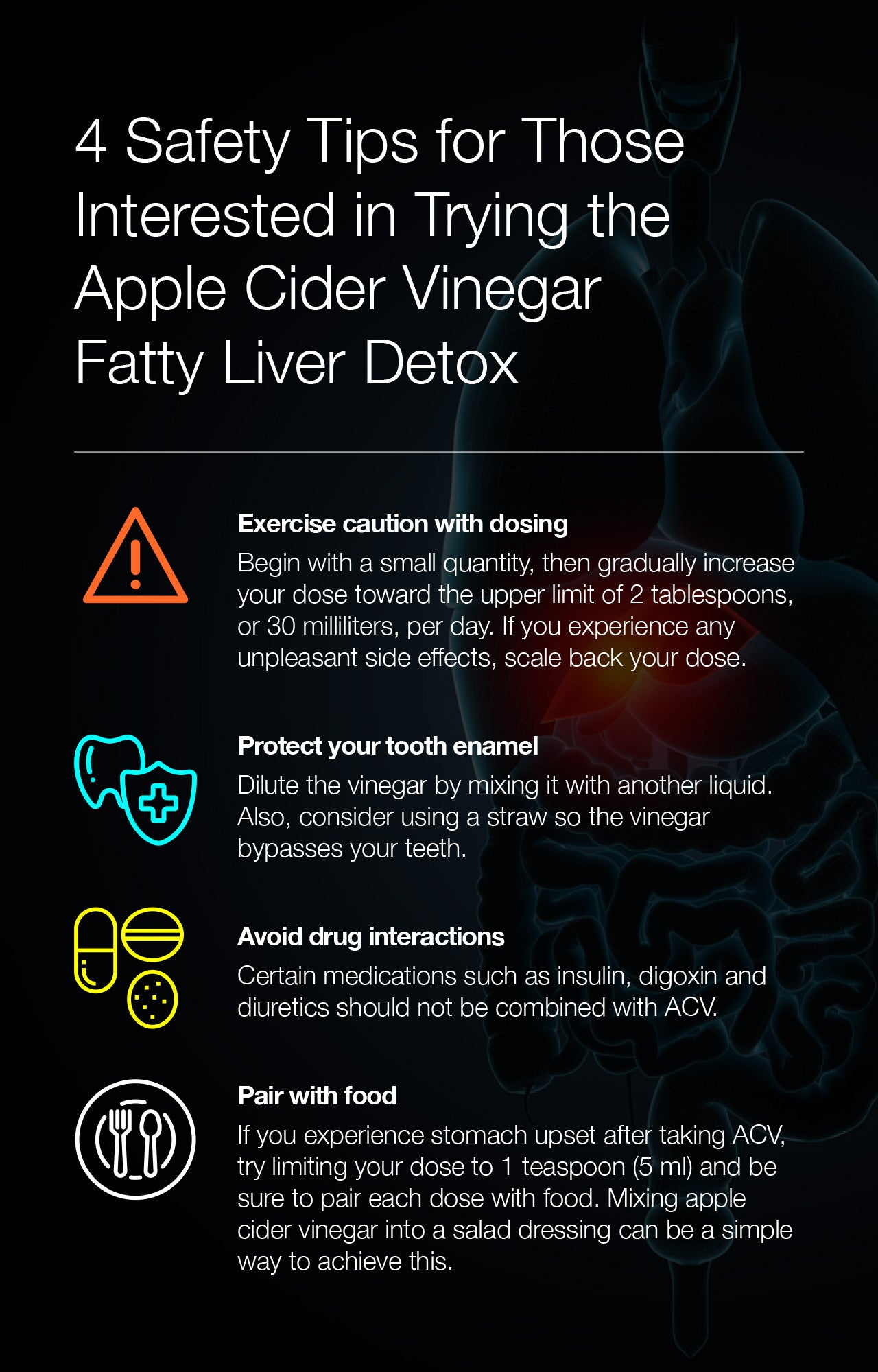
Given that there's no conclusive evidence to support the use of apple cider vinegar to treat fatty liver, those interested in trying this treatment should carefully weigh the potential negative side effects against the benefits they hope to achieve.
One of the most common issues associated with apple cider vinegar consumption is the erosion of tooth enamel. A 2014 study designed to evaluate the effects of different types of vinegar on tooth enamel found between 1% and 20% mineral loss (depending on the pH of the vinegar) after 4 hours of exposure. However, this study was done in a laboratory, so it's not entirely clear how those results would translate into real-life scenarios.
To be safe, those interested in adding ACV to their wellness routines should put one or more of following precautions in place:
- Carefully monitor the amounts consumed
- Mix with a glass of water
- Rinse mouth after drinking
- Use a straw
Because of its acidic nature, ACV has also been known to upset stomachs, yet another reason to dilute it in water. If you have a sensitive stomach, be sure to pair your doses of ACV with food.
It's also important to note that apple cider vinegar can interact with certain medications, such as insulin, digoxin, and diuretics. If you currently take prescription drugs, it's best to consult a doctor before taking ACV.
4 Proven Ways to Treat Fatty Liver Disease
While the evidence backing the use of the apple cider vinegar fatty liver detox can be characterized overall as weak, there are other natural methods for supporting and restoring liver health with much more robust scientific backing.
The best method for you will depend on the factors that have compromised your liver health, but it's likely to involve shifts to your diet, increased physical activity and, potentially, weight loss. There are also some supplements that have been shown to produce measurable improvements to liver health.
1. Diet
Research has shown that diet has a strong impact on your risk of developing many health conditions, including fatty liver disease. Certain foods can hinder liver health, such as:
- Trans fats
- Simple sugars
- Red meat
- Salt
- Fried foods
- Processed foods
Eating other foods, though, can bring about significant health benefits. In general, a good fatty liver diet will include plenty of high-fiber plant foods and very minimal amounts of sugar, salt, and both trans and saturated fats. Even if alcohol is not the root cause of your liver problems, it's essential to cut it out of your diet once your liver function has been harmed.
Those already dealing with liver problems, or interested in avoiding liver problems altogether, should be sure to include the following foods in their diets.
- Green vegetables, such as spinach, kale, and broccoli, which studies found prevented fat from accumulating in the liver
- Tofu, because soy protein has been shown to decrease fat buildup in the liver
- Omega-3 rich fish, like salmon, trout, and tuna, since scientists have discovered polyunsaturated fatty acids substantially improve liver health on multiple levels
- Nuts and seeds, especially sunflower seeds, which contain high levels of vitamin E, a powerful antioxidant proven to combat oxidative stress and halt the progression of liver disease
2. Physical Activity
To date, studies have shown that physical activity plays an overwhelmingly positive role in treating fatty liver disease. Per a 2018 review of 30 randomized controlled trials, "Physical inactivity is related to the severity of fatty liver disease irrespective of body weight." After reviewing the 30 trials, the authors concluded that data supports the common-sense conclusion that increasing physical activity improves liver health. It appears that exercise affects the development of fatty liver disease across multiple pathways.
Exercise has been shown to:
- Decrease insulin resistance
- Reduce excessive transport of fatty acids and glucose to the liver
- Increase fatty acid oxidation
- Decrease fatty acid synthesis
- Stymie the release of molecules that cause mitochondrial and hepatocellular damage
Both aerobic exercise and resistance exercise produce these positive effects.
3. Weight Loss
Carrying around excess body fat does elevate your risk of developing fatty liver disease. And conversely, losing even a small amount of weight can translate to major liver health improvements. According to a 2016 study, weight loss as achievable as 3% to 6% can decrease liver fat by between 35% and 40%.
4. Supplements
While lifestyle changes involving diet and physical activity produce the most profound effects on liver health, certain supplements do have scientifically validated liver health benefits. Three options we consider to be worthwhile are: milk thistle, turmeric, and amino acids.
Milk Thistle
This herbal remedy for fatty liver disease has potent anti-inflammatory, antioxidant, and antifibrotic (meaning, it reduces the formation of scar tissue) properties.
According to a study done by an Italian research team, silybin, the primary active compound found in milk thistle extract, has "a remarkable biological effect." It can reduce liver damage associated with chronic liver disease, cirrhosis, and hepatocellular carcinoma. It has also been shown to increase cellular vitality and decrease the accumulation of liver fat, oxidative stress, insulin resistance, and mitochondrial dysfunction.
Turmeric
According to a systematic review published in 2019, turmeric and its active compound curcumin may decrease the severity of nonalcoholic fatty liver disease. However, the authors note that all the trials they analyzed had small sample sizes, leading them to deem turmeric a "promising, but not proven" treatment for NAFLD.
A study published in Integrative Medicine Research in that same year looked specifically at the findings of randomized controlled trials on the use of turmeric and curcumin supplementation on NAFLD in adult patients. The primary outcomes analyzed were levels of two specific liver enzymes, alanine aminotransferase (ALT) and aspartate aminotransferase (AST). The meta-analysis, which included results from a combined total of 228 subjects, found a significant reduction of ALT concentrations among participants who took at least 1,000 milligrams of curcumin daily. This lead the researchers to conclude that high doses of curcumin appear to have a favorable effect on NAFLD, though further large-scale, high-quality studies should be done to confirm that effect.
Amino Acids
A wealth of research supports the benefits of regular amino acid supplementation for individuals who have fatty liver or who are at risk of developing the condition.
According to a 2018 study, taurine (a sulfur-containing amino acid) can prevent the accumulation of fatty acids in the livers of mice fed high-fat diets. Taurine also prevented oxidative damage and negative changes to liver enzyme levels. These effects led the study's authors to conclude that taurine could have "therapeutic value" for the treatment of nonalcoholic fatty liver disease.
A 2012 study, also done with mice, looked at the use of the three branched-chain amino acids (BCAAs) leucine, isoleucine, and valine. The researchers found that supplementing with BCAAs in the early stages of fatty liver disease can slow the progression of the disease—specifically, by decreasing liver fibrosis as well as liver cell death.
Another sulfur-containing amino acid, cysteine—available in supplement form as N-acetylcysteine (NAC)—has antioxidant properties to rival those of taurine. Per a 2010 clinical trial, participants who received NAC had significantly improved results in terms of levels of alanine aminotransfrase, aspartate aminotransfrase, and alkaline phosphatase as well as fat buildup and other measurements of liver function. Based on the results achieved at the 3-month mark, the researchers concluded that NAC can improve liver function in patients with non-alcoholic fatty liver disease, and that better results may be achievable with longer use.
Given what scientists have uncovered about the synergistic effects of amino acids, it's likely that the positive results achieved via supplementation with single amino acids could be amplified when taken in concert with an amino acid supplement that contains all nine essential amino acids. The essential amino acids work together to facilitate the body's biological processes, and providing a properly balanced supply of all the necessary building blocks not only safeguards and enhances the health of the liver, but also of the entire body.
Several studies have proven this true. A 2020 study published in the journal Nutrients showed that supplementation with a targeted high-dose of essential amino acids can help reduce excessive accumulation of lipids in the liver and offset the harmful effects of alcohol even when no other nutritional changes occur and alcohol consumption stays the same. And another study revealed that a 16-week supplementation regimen of 11 grams of amino acids a day with no changes to diet or physical activity levels resulted in a 50% reduction in liver fat content as well as significant improvements to triglyceride levels, total cholesterol, and very low density lipoprotein (VLDL).
You can start reversing fatty liver today with Amino Co's patented essential amino acid supplements designed to improve the health of your liver as well as your heart.

Exclusive Bonus: Download the FREE eBook that will show you how to start living your healthiest life.
Conclusion
Unsurprisingly, the high level of interest in natural remedies for fatty liver disease has led to the proliferation of some less than verifiable claims about certain treatment approaches.
While there's limited evidence to support the use of the apple cider vinegar fatty liver detox, the evidence that exists comes largely from studies done with animal subjects or with very limited enrollment. Plus, none of the studies focused specifically on the impact of ACV on liver health, but rather on effects related to linked health conditions such as excess body fat, high cholesterol levels, and poor blood sugar regulation.
It's also important to note that the apple cider vinegar fatty liver detox can have adverse side effects, such as the erosion of tooth enamel, stomach upset, and dangerous interactions with prescription drugs.
Given all that, the wisest choice is likely to try a natural treatment for fatty liver that has more substantial scientific backing. Effectively addressing fatty liver disease will likely require adopting a fatty liver diet and increasing your physical activity level, and may necessitate losing weight too. Incorporating supplements proven to improve liver health, like milk thistle, turmeric, and amino acids, can also be a valuable part of a fatty liver treatment plan.
An essential amino
acid-based formulation
Buy Now


Up to 25% off Amino
Shop NowTAGS: conditions liver natural cures
Join the Community
Comments (0)
Most Craveable Recipes




 833-264-6620
833-264-6620





















