Breast Cancer Screening Mammograms May Do More Harm Than Good
 By: by Amino Science
By: by Amino Science

Breast cancer is one of the most common types of cancer diagnosed in the United States. According to the non-profit organization BreastCancer.org, one in eight women in America will be diagnosed with an invasive breast cancer in her lifetime. Nearly 300,000 new cases of invasive breast cancer are expected to be diagnosed in American women in 2019, along with 62,930 cases of non-invasive breast cancer, which includes DCIS (ductal carcinoma in situ). It’s not only women who are affected by breast cancer. Although much less common in men than in women, there are over 2,270 new cases of invasive breast cancer expected in men in 2019.
Risk factors for breast cancer include age, gender, race, family history, and personal medical history. While these elements cannot be controlled, there are other factors that can be controlled to help reduce breast cancer risk or breast cancer recurrence. These include maintaining a nutritive diet and healthy weight, staying active, cutting back on the amount of alcohol consumed, quitting smoking, and limiting exposure to estrogen such as through birth control pills and hormone replacement therapy.
As with other forms of cancer, early detection is key when it comes to treating breast cancer. The earlier breast cancer is diagnosed, the more likely it can be treated and remission achieved. According to the American Cancer Society, women may begin annual breast cancer screenings at age 40, provided they have not had any previous instances of breast cancer or issues that may require them to begin screenings earlier than usual.
Breast cancer screening mammograms are the most common type of diagnostic test. Following is a breakdown of the mammogram, including what it is, how it works, the benefits of having it, and the potentially harmful side effects.
What Is a Mammogram?
While the test of screening for breast cancer in women is often called a mammogram, the mammogram itself is not the test. The mammogram is the x-ray image that the mammography test produces. In order to produce a mammogram, the mammography machine presses each breast between two plates and uses a low dose of radiation to take an x-ray image of each breast.
Although x-ray technology and screening mammography have existed since the late 19th and early 20th centuries, it was not until 1976 that the American Cancer Society began recommending mammography tests for the detection of breast cancer.
The current screening guidelines for women at average risk of breast cancer advise annual mammograms starting at age 45. Women ages 40-44 can opt for an annual mammogram, and at age 55 a mammogram every other year is typical health care protocol. But just because mammography is the most well-known and most common screening devise to detect breast cancer doesn’t necessarily mean that it is the most effective or the safest for all women.
Dangers of Mammograms
Mammograms have come under fire for producing false results leading to over-diagnosis and over-treatment, as well as for the pain and trauma inflicted on the breasts. Let's explore these complaints in more detail.
False Results
Mammograms have been known to produce both false-positive results and false-negative results. The false-positive results suggest that there is cancer present when there is not. A woman who receives a false-positive result will then undergo additional tests such as ultrasound and biopsy, which can cause emotional stress and anxiety as well as physical discomfort. Additional tests can also be expensive. According to the National Cancer Institute, 50% of women who have a mammogram every year for 10 years in the United States will receive a false-positive result and will then have a biopsy performed.
False-negative mammogram results occur when a mammogram does not detect cancer even though there is cancer present. This often occurs in women with dense breast tissue, as it is easier for cancer to hide in dense breast tissue than in fatty breast tissue. Women who receive a false-negative mammogram face a potentially life-threatening delay in treatment. The National Cancer Institute states that about 20% of mammograms being used to screen for breast cancer miss cancers that have already developed at the time of screening.
Over-Diagnosis and Over-Treatment
Mammograms cannot differentiate between different types of breast cancers. They can only show what appears to be cancer. This causes over-diagnosis and over-treatment.
Over-diagnosis and over-treatment occur when a type of breast cancer is found that is noninvasive, meaning it has not and will not spread to surrounding tissue. The cancer is isolated to that one spot in the breast and does not pose a threat. Other types of cancer are extremely slow growing and will not pose a risk to a woman’s health in her lifetime. Since mammograms cannot tell the difference between these types of cancers and more aggressive, invasive cancers, women often undergo unnecessary additional testing and even treatment such as chemotherapy or radiation for a cancer that was never going to grow, spread, or pose a health risk. According to women’s health expert Dr. Christiane Northrup, breast cancer over-diagnosis leads to unnecessary aggressive treatments, such as double mastectomies, for a cancer that was never going to threaten a woman’s life.
Pain and Trauma to the Breast
There’s no denying that getting a mammogram is not fun. While some women find them tolerable, other women find them extremely painful, especially women with any kind of scar tissue in the breasts. The pressing and squeezing of breasts can sometimes lead to bruising and physical trauma, particularly for women with breast implants. In rare cases, implants may even rupture during a mammography screening. Some women find mammograms so painful and uncomfortable that they skip mammograms or stop getting them altogether. Without regular screening for breast cancer, women are at a greater risk of a late diagnosis, which can lead to life-threatening illness and lengthy and costly treatments.
Improving Mammography
Mammography is making technological strides, as new strategies and breast cancer screening options are explored.
Since the turn of the century, digital mammography has typically been used over conventional mammography in most radiology practices. Both types of mammography use x-rays to take an image of the breast, but digital stores the electronic image as a computer file while conventional stores the image on film.
Beyond storage and sharing ease, digital mammography enables the radiologist to magnify and manipulate the image to better ascertain the results.
Digital breast tomosynthesis (DBT), or three-dimensional (3-D) mammography uses ex-rays to image the breast in thin strips and at different angles that are then reconstructed by computer software to form a complete picture. The drawback is the higher radiation dose. While DBT uses minimal dose x-rays, they're typically taken at the same time as standard digital mammography, which makes the total radiation dose higher than a standard breast screening test. It remains unclear whether 3-D mammography offers any advantages to detection or lower false-positive rates.
Health care providers are also using additional diagnostic tests to screen for breast cancer, such as magnetic resonance imaging (MRI), positron emission tomography(PET) scanning, and diffuse optical tomography, which uses light instead of x-rays for breast imaging.
A breast MRI is often the annual screening test of choice for women at high risk of breast cancer. It may also be used as a follow-up test if a clinical breast exam or mammogram showed an abnormal finding, or if the stage of breast cancer is yet to be determined.
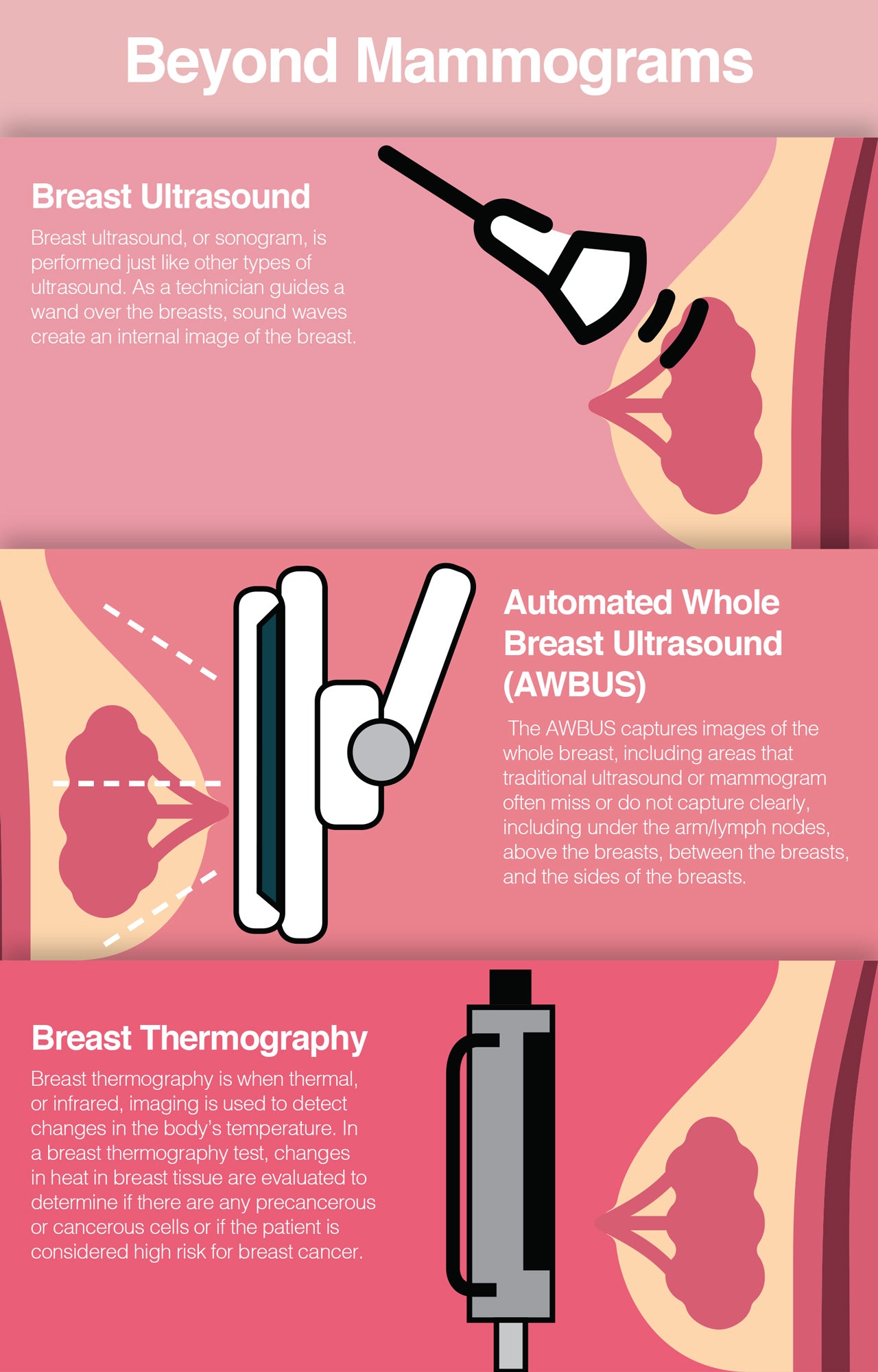
Beyond Mammograms
There are other options available for breast cancer screening beyond getting an annual mammogram that offer potential benefits, such as pain free and more appropriate for certain breast densities, although screening recommendations are still soundly in favor of mammography. Ultrasound, automated whole breast ultrasound, and thermography are a few noninvasive, painless options that can be added to an annual breast cancer screening routine.
Breast Ultrasound
Breast ultrasound, or sonogram, is performed just like other types of ultrasound. As a technician guides a wand over the breasts, sound waves create an internal image of the breast. Breast ultrasound is an option for women with dense breasts in particular as cancer can easily hide in dense tissue on a mammogram. Cancer stands out more clearly on an ultrasound than on a mammogram, making it more likely to be detected and treated.
Automated Whole Breast Ultrasound (AWBUS)
The SonoCine AWBUS was invented in 1999 by board-certified diagnostic radiologist Dr. Kevin Kelly of the Breast Ultrasound Center in Pasadena, California. Dr. Kelly realized the need for better diagnostic breast cancer tests, particularly for women with dense breast tissue.
The AWBUS captures images of the whole breast, including areas that traditional ultrasound or mammogram often miss or do not capture clearly, including under the arm/lymph nodes, above the breasts, between the breasts, and the sides of the breasts. The AWBUS can be used on all types of breasts including those that are mostly fatty tissue, mostly dense tissue, and breasts that have had cosmetic or reconstructive surgery. Like traditional handheld ultrasound, the AWBUS is painless and takes only a short amount of time to complete. It is also free of radiation, making it a safe option for pregnant and nursing women. Unlike traditional ultrasound, the AWBUS is automated, which eliminates technician error and offers consistent screenings for each patient.
Breast Thermography
Breast thermography uses thermal, or infrared, imaging to detect changes in the body’s temperature. In a breast thermography test, changes in heat in breast tissue are evaluated to determine if there are any precancerous or cancerous cells or if the patient is considered high risk for breast cancer. Breast thermography can often identify changes in breast tissue or cells that will likely lead to cancer before a tumor or growth is even present, unlike mammograms, which find cancer once a growth has already formed. Like ultrasound and AWBUS, breast thermography is pain-free and radiation free.
Every woman needs to decide for herself what route she is comfortable taking when it comes to breast cancer screening. While mammograms do detect cancer in the breast, they are not perfect and can yield false results. They can also result in painful and costly over diagnosis and over treatment as well as pain and trauma to the breasts from the actual mammography test.
Ultrasounds, whole breast ultrasounds, and breast thermography may not be enough to replace an annual mammogram, but they are great options when it comes to taking additional steps to protect your breasts from cancer risk and potential risks from mammograms. It is important to stay informed about the downside of mammograms, who should be getting additional screening such as women with dense breast tissue, and what other screening options are available.
To support overall health and wellness and protect against chronic diseases such as breast cancer, we recommend Amino Co's Active Aging Blend. You can learn all about Life here.

Up to 25% off Amino
Shop NowTAGS: anti-aging conditions
Join the Community
Comments (0)
Most Craveable Recipes



 833-264-6620
833-264-6620